All published articles of this journal are available on ScienceDirect.
A Systematic Review of Pain Assessment in Mechanically Ventilated Patients
Abstract
Introduction:
Pain self-report is the gold standard of pain assessment. Mechanically ventilated patients cannot self-report the pain due to the presence of a tracheal tube and changes in the level of consciousness caused by sedation, exposing them to the risk of inadequate pain management that leads to psychological and physiological consequences. This study aimed to present a review of the published evidence and studies concerning the scales used in pain assessment in mechanically ventilated patients according to their psychometric characteristics and application in the nursing practice.
Methods:
We conducted a systematic review following PRISMA guidelines. National and international journals in such databases as Science Direct, PubMed, EMBASE, Pro Quest Central, Web of Science, SID, and Magiran were searched using Persian and English keywords, and retrieved articles were included in this review based on the inclusion and exclusion criteria.
Results:
22 articles were included in this review based on the inclusion and exclusion criteria. According to the research objectives, findings were extracted from selected articles and reviewed in two sections: 1] validity and reliability, and 2] clinical application.
Conclusion:
Scales of CPOT and BPS are superior to NVPS, and a combination of BPS and CPOT improves the pain detection accuracy, and vital symptoms should be used cautiously for pain assessment along with objective measures due to poor evidence. Moreover, rapid and effective pain relief plays an important role in the improvement of psychological and physiological consequences.
1. INTRODUCTION
Of over 5,000,000 patients hospitalized annually in the intensive care unit (ICU), more than 53% require mechanical ventilation [1]. Despite the fact that pain has been studied in mechanically ventilated patients during the last 20 years [2], about 80% of patients experience moderate to severe pain [3]. Pain is referred to as the most unpleasant memory of patients at the time of discharge from ICUs and even 5 years post-discharge [4, 5]. Existing reports indicate that more than 80% of ICU patients mention their painful memories and distress about the tracheal tube [6]. These patients also perceive pain at times of routine care procedures and even while resting [5-8].
Patient conditions and some factors in ICUs, including endotracheal intubation, mechanical ventilation, reduction of consciousness level, sedation, and administration of relaxing drugs, can change verbal communication and make pain assessment difficult [9]. Mechanically ventilated patients cannot self-report the pain due to the presence of tracheal tube and changes in the level of consciousness caused by sedation [5, 8], exposing them to the risk of inadequate pain management [10].
The first essential step in pain control is the assessment [7], that is, a reliable assessment tool is necessary for effective pain management. Such a tool can help make a correct decision at the time of pain management and improve pain detection and assessment [11]. Due to the subjective nature of pain, self-report is a gold standard for pain assessment [12, 13]. The commonly used pain scales include numerical rating scale (NRS) and visual analog scale (VAS) [6], and this method is not adequate in ICU patients due to the presence of communicative disorders [7]. In the absence of pain self-report, observational scales can replace pain assessment methods [14]. One of the pain indicators traditionally used in nonverbal patients is changes in vital signs. However, relying on changes in vital signs as a major indicator of pain can be misleading, as these changes may be influenced by other factors such as underlying physiological conditions and medications. Thus, changes in vital symptoms are not good indices for pain assessment but are often a guide for further assessment of pain [5, 15]. In nonverbal patients, therefore, behavioral pain scales are an alternative to self-reported pain [4, 12, 16]. Pain scales can also be one-dimensional or multi-dimensional, with the former consisting of behavioral responses and the latter comprising physiological responses or instructions for making therapeutic decisions and assessing a patient’s ability intolerance to narcotics, in addition to behavioral responses. Of nine reliable scales for adult patients, six and three scales are one- and multi-dimensional, respectively [2]. Behavioral Pain Scale (BPS), Critical Care Pain Observational Tool (CPOT), and Pain Behavior Assessment Tool (PBAT) are the most common one-dimensional scales, and Nonverbal Pain Scale (NVPS) and Pain Assessment and Intervention Notation (PAIN) Algorithm are the most widespread multi-dimensional scales [17].
Inadequate control and non-treatment of pain are associated with psychological and physiological consequences [18, 19] and can affect the endocrine, cardiovascular, immune, nervous, and musculoskeletal systems [9]. This results in adverse consequences, including hyperglycemia, chronic pain syndrome, prolonged hospitalization, hypertension, tachycardia, increased oxygen demand, decreased perfusion, anxiety, impaired mobility and sleep, prolonged mechanical ventilation, immune system malfunction, impaired wound healing, coagulopathies, and respiratory dysfunction [6, 9, 13, 18, 20]. Granja et al. also reported that 18% of ICU patients were at the risk of Post-Traumatic Stress Disorder (PTSD) [6].
A well-controlled pain of patients will lead to desirable consequences, including decreased duration of mechanical ventilation and ICU stays, declined need for painkillers and sedatives, reduction of nosocomial infections and mortality, improved quality of life, and increased patient satisfaction [7, 15, 18]. Daily management cost for an ICU patient is estimated to be $ 3000-4000, and mechanical ventilation can add up to $ 1500 to this cost. Pain control, therefore, has a major effect on patient recovery and medical costs [18]. Based on these positive results, pain assessment is deemed as a strategy for better care in ICUs [2]. Although mechanical ventilation is a life-maintaining intervention, it is not void of complications [such as ventilator-associated pneumonia and deep vein thrombosis] [11]. Separation from mechanical ventilation should be started in ICU patients as soon as possible to prevent ventilator-associated events, and inadequate pain management can preclude the separation of the patient from mechanical ventilation [6]. Furthermore, most patients require some levels of sedation in the early days after intubation. Factors such as the presence of tracheal tube, verbal impairment, non-coordination of patients with the ventilator, and frequent need to use physical restraints have been shown to play a role in the distress of mechanically ventilated patients. For a long time, nurses provided patients with convenience using high levels of sedatives and muscle relaxants to increase their tolerance to the ventilator. However, excessive and prolonged sedation has been demonstrated to result in delayed recovery and negative consequences, including prolonged mechanical ventilation and increased ICU stays [7, 11]. Therefore, it is recommended to avoid excessive administration of sedatives and analgesics in order to reduce the duration of mechanical ventilation. These recommendations highlight the importance of an accurate pain assessment in mechanically ventilated patients [1, 8]. This is because an accurate pain assessment will be associated with the appropriate administration of sedatives and analgesics and will result in consequences as reduction of complications and early separation from the mechanical ventilator [1].
2. OBJECTIVES
Given the importance of pain detection and assessment, the review questions for this study were as follows. (a) What does the literature report about the psychometric properties of the tools used in pain assessment in mechanically ventilated patients? (b) What does the literature say about their application in nursing practice?
3. METHODS
This systematic review has been conducted through the collection and review of documentation, articles, and resources available in 2020.
International databases, namely Science Direct, PubMed, EMBASE, Pro Quest Central, and Web of Science, as well as Persian databases (SID and Magiran) were searched to find articles through a systematic search method using Persian and English keywords and possible Mesh-based combination without time limitation. Some Persian and English keywords used in the search were pain, pain assessment, pain management, and mechanical ventilation.
Patients aged > 16 years undergoing mechanical ventilation, application and/or psychometric characteristics of tools, research tools including BPS, CPOT, and NVPS, original studies published in peer -review journals, and full- text availability were the inclusion criteria. Patients aged < 16 years undergoing mechanical ventilation, studies using other scales for pain assessment, gray literature, letters, editorials, commentaries, review articles, and those presented at seminars and conferences and also PBAT tool this tool is not designed as a scoring tool, and pain management decisions are based on nurses' clinical judgment with this tool [12] were excluded from this review.
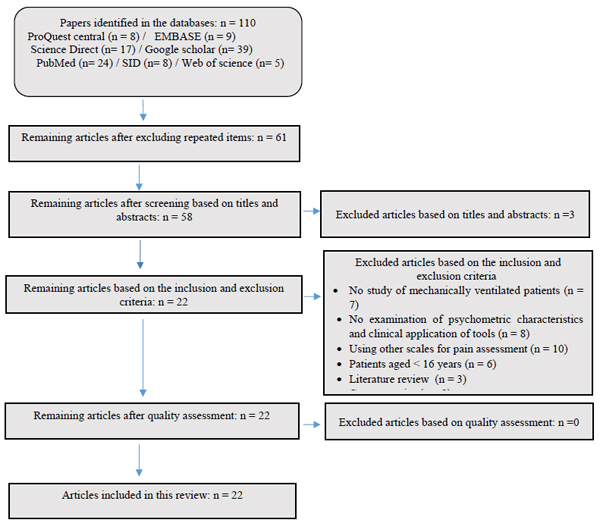
Two researchers familiar with a systematic search method carried out the search from September 2020 to December 2020 according to the targeted keywords and databases and then documented the search details. Fig. (1) summarizes the details of 110 articles found here.
49 repetitive articles identified by the EndNote software were excluded from the study. The same two researchers reviewed the abstracts, who omitted unrelated articles and determined those related to this study to receive the full texts and extract data, and finally 22 articles were included in this review. To reduce human errors, the two researchers separately, according to a checklist (Table 1), extracted predetermined required data, and the two results were matched to each other. The quality of data collected by the checklist was assessed by two other experts, and the names of journals and authors were omitted to avoid bias.
4. ANALYSIS
We extracted and grouped the results according to the research question from 22 studies. The main statements from the findings that represent psychometric properties of pain instruments and their application in nursing practice were noted down as evidence and classified into two major topics. The retrieved 22 articles were published from 2010 to 2019, with three in the United States and the Netherlands, five in Canada, one in Iran, Turkey, Germany, Saudi Arabia, Italy, Finland, and Thailand, and two in Poland and China. The articles were descriptive, methodological, cross-sectional, and pre-and post-interventional designs.
5. RESULTS
According to the study objectives, the findings are described below, and the details of results and scales are shown in Tables 2 and 3, respectively.
5.1. The Validity and Reliability of Tools used in Mechanically Ventilated Patients
The psychometric characteristics of the NVPS were examined in four out of 22 studies [13-16]. The internal consistency of tools was reported with Cronbach’s alphas of 0.75, 0.77, and 0.8 in three studies [13, 15, 16]. Inter-rater reliability was reported with ICC=0.92 and ICC = 0.68 in two surveys [14, 15], and with a Pearson correlation of 0.89-0.96 in another study [13]. Discriminant validity was shown with significant differences in pain scores during painful (change of position) and non-painful procedures (eyewash with normal saline and blood pressure cuff) [13, 14], at rest and after the change of position [15], as well as during suction before and after the procedure [16] (P < 0.001). The studies concluded that there were good and reliable psychometric characteristics in NVPS for pain assessment in mechanically ventilated patients.
Three of the 22 studies focused on the psychometric characteristics of BPS [17-19] and reported ICC = 0.87 [17], ICC = 0.86 [18], and ICC = 0.981 [19] in their results, indicating good inter-rater reliability. Three surveys presented the discriminant validity with increasing pain scores during painful procedures relative to those before and after painful procedures [18], increasing pain scores during painful procedures relative to non-painful ones (P < 0.001) [19], and increasing pain scores before (Interquartile range (IQR) BPS = 5) and after (IQR BPS = 4) painkiller administration [17]. Criterion validity was observed with good to strong Pearson correlations between NRS and BPS scores in two studies (r > 0.57, P < 0.00001; r = 0.815-0.937) [18, 19]. In two studies, internal consistency was reported with Cronbach’s alphas of 0.724-0.743 [19] and 0.79-0.81 [17].
Seven out of the 22 studies examined the reliability and validity of the CPOT scale [14, 17, 20-24]. In four studies, internal consistency was reported with Cronbach’s alphas of 0.79-0.81 [17], 0.56 [21], 0.79 [23], and 0.86 [22]. Inter-rater reliability was reported from good to medium (ICC = 0.38 at rest and ICC = 0.56 in a change of position) [24] in one study, but it was reported to be very excellent in three other surveys (ICC ≥ 0.91) [17, 20, 22], and with a high Pearson correlation (r = 0.72) in another investigation [23]. In two studies, inter-rater reliability was reported to be lower at rest than in painful procedures, suggesting the dependability of CPOT in the assessments of body and face postures in response to therapeutic procedures [20, 21]. In one study, the criterion validity was analyzed by calculating the sensitivity and specificity of CPOT scores using patients’ self-reports as a standard reference, and values of 0.39 and 0.85 were expressed for the sensitivity and specificity of CPOT respectively, with a threshold of 2 [21]. In three studies, the criteria validity was presented with positive medium Pearson correlations of r = 0.435 and r = 0.574–0.705 (P < 0.001) in two investigations [14, 22] and excellent (r = 0.91) in the other one [23]. In five surveys, the Criterion validity was reported with increasing pain scores during painful procedures relative to non-painful ones (P < 0.001) [14, 20, 22], during painful procedures (change of position) relative to at rest (P < 0.001 [23], and with increasing pain scores before (IQR CPOT = 3) and after (IQR CPOT = 1-2) painkiller administration [17]. The studies concluded that the CPOT was a reliable and valid tool for pain detection during oral care measures [20].
Four out of the 22 surveys compared psychometric characteristics of CPOT and BPS scales [5, 25-27]. In one study, mean scores of CPOT and BPS increased by 2 points in painful procedures compared with those of rest modes (CPOT 0-2, P = 0.000; BPS 3-5 P = 0.000), and mean scores of BPS increased significantly from 1 score between the rest and non-painful procedures while those of CPOT remained unchanged (BPS 3.0-4.0, P = 0.002; CPOT 0.0-0.0, P = 0.000) [25]. In another research, mean scores of CPOT and BPS for both nurses increased significantly by 2 points from rest 2 to change of position, and mean scores of BPS between rest 1 and non-painful procedures (oral care) increased significantly by 0.5 points for nurse 1, while those for nurse 2 and CPOT scores of both nurses remained unchanged. These increases in the scores during oral care mainly occurred due to gaining higher scores in components of facial expressions and upper extremity movements [26]. Three studies reported Cronbach’s alphas of 0.70 and 0.71 (acceptable internal consistency) for BPS and CPOT [25], less than 0.70 (for both tools) [26], and 0.921 and 0.950 (high internal consistency), respectively [27]. In two investigations, high correlations were observed between the two scales in painful procedures (Cohen’s Kappa = 0.64 [5] and r =0.906 [27]), suggesting a greater tendency of both tools in the reflection of pain sensitivity [27]. Inter-rater reliability was reported from relatively good to good in two studies (BPS ICC=0.74, CPOT ICC= 0.75 [25] and CPOT & BPS ICC=0.74 [26]). According to results, BPS increased more significantly than CPOT during non-painful procedures, and discriminant validity supported the use of BPS to a lower extent, as it increased during non-painful procedures [25, 26].
Three out of the 22 surveys compared the psychometric characteristics of CPOT, and BPS, and NVPS scales [24, 28, 29]. In one study, good results were obtained in the internal consistency of scales, but CPOT and NVPS were better than BPS (0.96, 0.90, and 0.86, respectively), and NVPS showed better reliability among inter-raters than the other two scales; however, these scales were considered to be reliable [28]. In another survey, all the three scales displayed good psychometric characteristics but CPOT and BPS were better than NVPS in terms of inter-rater reliability and internal consistency (Cronbach’s alphas of 0.8, 0.81, and 0.76 for BPS, CPOT, and NVPS, respectively) [24]. Similarly, another research presented evidence that CPOT and BPS scales (both with a Cronbach’s alpha of 0.95) had better reliability than NVPS (Cronbach’s alpha = 0.86). The least agreement between inter-raters for NVPS and BPS was identified in facial expressions (NVPS r = 0.72, BPS r = 0.77) and in muscular tension (r = 0.47) for CPOT. It was concluded that BPS had the highest validity and reliability and, together with CPOT, was considered as suitable alternative scale for pain assessment. NVPS was not recommended due to poor psychometric characteristics, particularly in physiology and respiratory components [29]. In another investigation on psychometric characteristics of CPOT and NVPS, the former was found to have better reliability than the latter for pain assessment in patients without the ability of verbal communication [14]. In a study on psychometric characteristics of BPS and NVPS, internal consistency was reported to be less than 0.7 for both scales (Cronbach’s alphas of 0.6883 and 0.6697 for BPS and NVPS, respectively). The internal consistency of NVPS was lower than BPS, and discriminant validity was not confirmed for NVPS. It was concluded that BPS had better psychometric characteristics than NVPS [30].
Three out of the 22 surveys highlighted the specificity and sensitivity of tools [5, 17, 23]. In one study, the specificity of tools (0.847 and 0.679 for CPOT and BPS, respectively) was higher than the sensitivity (0.643 and 0.672 for CPOT and BPS, respectively), leading to positive predictive values of 82.9% and 77.2% for CPOT and BPS, respectively. In other words, 82.9% and 77.2% of patients diagnosed with pain scores of CPOT > 2 and BPS > 4, respectively, underwent pain treatment [17]. In another study, particularly in nursing care procedures, low sensitivity and specificity were found for BPS (specificity = 91.7%, sensitivity = 62.8%, and accuracy = 72.04%) and CPOT (specificity = 70.8%, sensitivity = 76.5%, and accuracy = 74.68%), and a combination of the two tools was observed to show better sensitivity (80.4%) [5]. In another study, For CPOT > 2, values of 93% and 84% were reported for sensitivity and specificity, with a positive predictive value of 85% [23].
5.2. Feasibility and Clinical Application of Scales used in Mechanically Ventilated Patients
Feasibility and clinical application of scales were investigated in eight out of the 22 studies. In one study, BPS and NVPS scales were easier to learn than CPOT, and memorization of BPS was reported to be easier than the other scales. The tools were not significantly different in terms of accuracy and utility, and NVPS (43%) was often reported as the preferred tool, followed by BPS (33%) and CPOT (24%) [24]. In another study, on the other hand, CPOT was more acceptable among nurses than NVPS, and CPOT was found to be a useful scale in the detection and assessment of pain signs in patients incapable of verbal communication [14]. Similarly, an easy understanding and completion of CPOT were found in two investigations, and, according to the reports, more than 70% of nurses believed that the use of CPOT was helpful in nursing practice and was recommended to be used routinely [31, 32]. CPOT also affected the communication of nurses (78.3%), leading to the transfer of pain assessment results to other nurses [32]. In another research, 78% of nurses stated that NVPS scale was easy to apply and its implementation was associated with nurses’ consent of pain management strategy in ICU (P = 0.04), increased patient satisfaction and documentation of pain assessment [33]. A study compared the feasibility of CPOT and BPS scales and found no significant differences among nurses’ understanding of the feasibility and satisfaction in the use of BPS compared with CPOT. Although there were no significant differences, the mean scores of CPOT were slightly higher than those of BPS in terms of feasibility and satisfaction [27]. In a similar investigation on the feasibility assessment of CPOT, nurses were highly satisfied with its clinical application (85% of answers 4 or 5 in the Likert scale) [23]. However, another research showed that BPS was superior to CPOT in all criteria and that BPS was a more practical pain scale for application in a clinical setting than CPOT, specifically because it required less time for application [17].
| Ref. | Country | Type of Study | Objective |
|---|---|---|---|
| Topolovec-Vranic [14] 2013 | Canada | Prospective descriptive | Evaluation of validity and clinical application of two pain assessment tools (NVPS-R and CPOT0 in trauma and neurosurgery patients |
| Juarez [15] 2010 |
United States | Methodological | Evaluation of validity and reliability of two pain assessment tools (BPS, NVPS) in adult mechanically ventilated patients |
| Heidarzadeh [13] 2018 |
Iran | Methodological | Evaluation of psychometric properties of NVPS in mechanically ventilated patients in intensive care units |
| Kaya [16] 2018 |
Turkey | Methodological | Evaluation of validity and reliability of the NVPS-R tool in intensive care units |
| Wongtangman [17] 2017 |
Thailand | Prospective descriptive | Evaluation of psychometric properties of CPOT and BPS in postoperative mechanically ventilated patients in intensive care units |
| Kotfis [18] 2018 |
Poland | Cohort, Observational Prospective | Validity of the Polish version of the BPS scale in mechanically ventilated patients and sedation with morphine and dexmedetomidine after cardiac surgery |
| Chen [19] 2016 |
China | Cross-sectional | The validity and reliability of the Chinese version of BPS for intubated patients and BPS-NI for non-intubated patients in intensive care units |
| Craig [20] 2018 |
Canada | Observational Prospective | Evaluation of the validity and reliability of CPOT for the diagnosis of oral-pharyngeal pain in intubated and tracheostomy adult patients during oral care procedures |
| Stilma [21] 2015 |
Netherlands | Observational Cross-sectional |
Validation of the Dutch version of CPOT in mechanically ventilated patients in intensive care units |
| Chen [22] 2019 |
China | Cross-sectional | The validity and reliability of the Chinese version of CPOT in intubated and non-intubated patients in intensive care units |
| Emsden [23] 2019 |
Germany | Observational | Evaluation of the validity and reliability of the German version of CPOT and its feasibility in clinical operations in intensive care units |
| Chanques [24] 2014 |
United States | Psychometric tool | Comparison of psychometric properties of three pain tools (BPS, CPOT, and NVPS) in critically ill patients lacking the self-report ability |
| Rijkenberg [25] 2014 |
Netherlands | Cohort, Observational Prospective | Comparison of the validity and reliability of CPOT and BPS tools in mechanically ventilated patients in intensive care units |
| Rijkenberg [26] 2017 |
Netherlands | Cohort, Observational Prospective | Comparison of the validity and reliability of CPOT and BPS tools in postoperative mechanically ventilated patients |
| Weldon [27] 2017 |
United States | Correlational and comparative | Evaluation and comparison of CPOT and BPS tools in effective detection of pain and their feasibility in mechanically ventilated patients |
| Severgnini [5] 2016 |
Italy | Observational Prospective | Evaluation and comparison of CPOT and BPS tools in conscious and unconscious mechanically ventilated patients |
| Tähkä [28] 2018 |
Finland | Psychometric tool | Validity of the Finnish version of pain tools [CPOT, NVPS, and BPS] in sedated patients in intensive care units |
| Al Darwish [29] 2016 |
Saudi Arabia | Descriptive | Finding the most reliable, sensitive, and authentic pain tools among CPOT, NVPS, and BPS tools in mechanically ventilated patients |
| Wojnicka [30] 2019 |
Poland | Descriptive Prospective |
Evaluation of psychometric properties of BPS and NVPS tools in mechanically ventilated patients |
| Gélinas [31] 2010 |
Canada | Descriptive | Nurses' assessment of the feasibility and clinical application of CPOT tool in mechanically ventilated patients |
| Gélinas [32] 2014 |
Canada | Descriptive | Nurses' evaluation of feasibility, clinical relevance, and satisfaction with CPOT use at 12 months after implementation |
| Topolovec- Vranic [33] 2010 | Canada | Pre- and post-intervention | Evaluation of the effect of implementing a new pain assessment tool NVPS in trauma/neurosurgery intensive care units |
| Validity and Reliability of Tools | |||||||
|---|---|---|---|---|---|---|---|
| - | NVPS | BPS | CPOT | ||||
| The internal consistency (Cronbach’s alphas) | > 0.75 in five studies and less than 0.70 in one study, also it was reported 0.90 in one study | > 0.7 in six studies and less than 0.70 in two studies, also it was reported 0.950 in two studies |
> 0.56 in five studies and less than 0.70 in one study but in two other study was good (>0.94) |
||||
| Inter-rater reliability (Intraclass Correlation Coefficient) | ICC > 0.68 in two studies | ICC > 0.86 in three studies ICC=0.74 in two studies |
ICC = 0.56 in one study, but it was reported to be very excellent in three other surveys (ICC ≥ 0.91) ICC> 0.74 in two studies |
||||
| Specificity | 0.67 and 0.91 in two studies | 0.70 in one study and 0.84 in two studies | |||||
| Sensitivity | 0.67 and 0.62 in two studies | 0.64, 0.93 and 0.76 in three studies | |||||
| Feasibility and Clinical Application of Scales | |||||||
| • CPOT is a useful scale in the detection and assessment of pain signs in patients incapable of verbal communication; also, nurses were highly satisfied with its clinical application. • Memorization of BPS is easier than the other scales. • Easy understanding and completion of CPOT and BPS. • Implementation of NVPS was associated with nurses’ consent in pain management. |
|||||||
| Tool | Score | Domain | |||||
| Behavioral Pain Scale (BPS) | Each domain: 1–4 Total score: 3 (no pain) to 12 (most pain) | Facial expressions | 3 | 1 | |||
| Partially tightened | 2 | ||||||
| Fully tightened | 3 | ||||||
| Grimacing | 4 | ||||||
| Compliance with ventilation | Tolerating movements | 1 | |||||
| Coughing but tolerating | 2 | ||||||
| Fighting ventilator | 3 | ||||||
| Unable to control ventilation | 4 | ||||||
| Movement of upper limbs | No movement | 1 | |||||
| Partially bent | 2 | ||||||
| Fully bent | 3 | ||||||
| Permanently retracted | 4 | ||||||
| Critical-Care Pain Observation Tool (CPOT) | Each domain: 0–2 Total score: 0 (no pain) to 8 (most pain) | Facial expressions | Relaxed, neutral | 0 | |||
| Tense | 1 | ||||||
| Grimacing | 2 | ||||||
| Body movements | Absence of movements | 0 | |||||
| Protection | 1 | ||||||
| Restlessness | 2 | ||||||
| Muscle tension | Relaxed | 0 | |||||
| Tense, rigid | 1 | ||||||
| Very tense | 2 | ||||||
| Ventilator compliance | Tolerating ventilator | 0 | |||||
| Coughing but tolerating | 1 | ||||||
| Fighting ventilator | 2 | ||||||
| Nonverbal Pain Scale (NVPS) | Each domain: 0–2 Total score: 0 (no pain) to 10 (most pain) | Face | No particular expression or smile | 0 | |||
| Occasional grimace, tearing, frowning forehead | 1 | ||||||
| Frequent grimace, tearing, frowning forehead | 2 | ||||||
| Activity | Lying quietly, normal position | 0 | |||||
| Seeking attention through the movement of slow, cautious movement | 1 | ||||||
| Restless activity and/or withdrawal reflexes | 2 | ||||||
| Guarding | Lying quietly, no positioning of hands over areas of the body | 0 | |||||
| Splinting areas of the body, tense | 1 | ||||||
| Rigid, stiff | 2 | ||||||
| Physiology (vital signs) | Stable vital signs, no change in past 4 hours | 0 | |||||
| Change over the past 4 hours in any of the following: SBP1 >20, HR2 >20 |
1 | ||||||
| Change over the past 4 hours in any of the following: SBP >30, HR >25 | 2 | ||||||
| Respiratory | Baseline RR3/SpO24 Complaint with ventilator | 0 | |||||
| RR >10 above baseline or 5% ↓ SpO2 Mild asynchrony with ventilator | 1 | ||||||
| RR >20 above baseline or 10% ↓ SpO2 Severe asynchrony with ventilator | 2 | ||||||
6. DISCUSSION
The development of strategies for minimizing psychophysical distresses and unpleasant memories concerning tracheal tube and mechanical ventilation is one of the priorities in nursing care [34]. The use of behavioral pain scales is one of the strategies to improve pain assessment in mechanically ventilated adult patients who cannot evaluate their pain levels [15].
Robleda, Ayasrah, and Chanques respectively reported that 61, 33.2, and 63% of patients suffered from pain at rest (BPS score > 3). Such a high percentage highlights that pain remains a real problem in ICUs [4, 35, 36]. Robleda reported that pain at rest was a risk factor for pain exacerbation during procedures. Accordingly, the authors emphasized that good pain management at rest might lead to pain reduction during procedures [4]. Physicians, therefore, should bear in mind that even safe and convenient measures may be painful for patients and should accurately evaluate care-related pain during patient care to improve health care quality [35].
There were discrepancies for determining the best scale in studies that investigated and compared the reliability and validity of BPS, CPOT, and NVPS scales, with the first two scales having better reliability and internal consistency than NVPS [8, 24]. Based on a report by Chookolaie et al. (2017), CPOT had good psychometric characteristics in non-verbal patients hospitalized in ICUs, with RASS scores from −3 to +1, but it was not a good scale for pain assessment in agitated patients according to RASS [37]. Rijkenberg et al. observed a significant increase in BPS scores during non-painful procedures, and the highest score resulted from changes in facial expressions and upper limb movements. This increased score of facial expressions during non-painful procedures was an automatic response to palpation, not to pain [25]. According to Tássia (2020), therefore, most pain scales have satisfactory validity and reliability and, despite a decrease in the number of scientific articles in this field, BPS and CPOT scales have good psychometric characteristics. However, sufficient data are not available to be able to demonstrate the superior pain assessment scales in ICUs [8].
The application of CPOT and NVPS in nonverbal patients was reported to be associated with improved patients' perceptions of pain, pain documentation, nurses' self-confidence in pain assessment, increased frequency of pain assessment, and decreased use of sedatives [2, 38, 39]. In studies by Louise and Damico (2018), the application of CPOT using appropriate training and resources was associated with increased use of analgesics, which was attributed to an increased number of clinical therapeutic interventions to mitigate patients’ pain [40, 41]. In Rose et al. (2013), on the other hand, the application of CPOT increased the frequency of pain assessment after the implementation in comparison to before the execution; however, approx. 40% of the incidence of pain was not associated with the administration of analgesics. Hence, it is important for nurses to respond to pain assessment findings by appropriate interventions for pain relief [32]. It can be concluded that the use of CPOT increases the sensitivity of nurses to pain, directs them towards pain management and control, and is a suitable scale for pain assessment in mechanically ventilated patients [8, 42]. CPOT was more acceptable than NVPS in studies on the clinical application of these two pain assessment scales, and 73% of nurses stated that the use of CPOT was effective in nursing practice [8, 10]. Deborah (2010) and Fothergill (2016) reported that Nonverbal Pain Assessment Tool (NPAT) and CPOT were easy-to-use and paved the ground for the effectiveness of interventions and pain documentation [43, 44]. Therefore, the ease of use and the team familiarity should be considered when making decisions on the use of pain assessment scales [8]. Since BPS and CPOT are easy to use, they can also be used by family members [45].
In Severgnini et al., BPS was reported to have greater specificity but lower sensitivity than CPOT, and a combination of the two scales led to a better sensitivity [80.4%] in pain detection [5]. Similarly, Kiavar found that an agreement between CPOT and pain-induced physiological changes was greater than FE, indicating higher sensitivity of the former than the latter scale [9]. Marmo et al. also detected that CPOT was a more sensitive scale than the other two scales (FLACC and NVPS) [46]. It can, therefore, be concluded that CPOT and BPS, with different sensitivity and specificity, can be used for pain intensity assessment in mechanically ventilated patients. In addition, a combination of CPOT and BPS improves pain detection accuracy in comparison to individual use of the scales [5, 9]. Robleda and Barzanji (2016) and Shan (2018) reported that the Bispectral index (BIS) and CPOT scales had better sensitivity to vital symptoms, suggesting that vital symptoms cannot be used alone for pain assessment in paints that are not able to report pain. This is because vital symptoms are not pain-specific and can be influenced by drugs (e.g., vasopressors, beta-blockers, and anti-arrhythmia factors) or an underlying disease (sepsis), which can somewhat inhibit physiological responses [2, 4, 45, 47]. Erden et al. (2017) observed a positive correlation between pain intensity with heart rate and respiration. However, their results emphasized that hemodynamic changes for pain assessment were not always an accurate measurement in patients and did not manifest unchanged vital symptoms of painlessness; hence, they should be used with other reliable pain assessment scales (e.g., NRS or BPS), depending on patients’ consciousness status [48]. Furthermore, catecholamines have a short biological half-life and are metabolized rapidly; thus a decrease in the heart rate and mean arterial pressure 20 min after suction may occur due to the metabolism of catecholamine and does not mean pain relief [49]. Given the poor evidence about vital symptoms, therefore, they should be used cautiously together with objective measures (behavioral scales) for pain assessment. Shan also reported that BIS was more appropriate for pain assessment in patients with severe consciousness disorder and that a combination of CPOT and BIS had more sensitivity in pain detection. Thus, changes in BIS may provide useful information about pain, but further research is necessary [47].
In studies by Deldar and Louise, unfamiliarity with pain assessment scales and lack of appropriate tools in nonverbal patients were identified as the major barriers to pain assessment [40, 50]. Topolovec-Vranic et al. reported that the lack of interest in the use of a new assessment scale was another major barrier to pain assessment, which was attributed to different factors, including resistance to change, understanding of excessive workload, or lack of data about positive effects of scales [33]. Additionally, Rose et al. (2012) investigated the performance of nurses regarding pain control and management. They reported that nurses were not interested in using pain assessment scales in nonverbal patients and had little information on such scales, which could negatively affect pain management [51]. Therefore, barriers to the use of pain assessment scales lead to inaccurate assessment and thus unreal pain perception and administration of inadequate analgesics. Accordingly, the identification of these challenges in nurses can help to empower them in the use of behavioral pain assessment scales, pain relief, and quality improvement of care services [50].
7. LIMITATIONS
This systematic review included resources that were published in peer-reviewed journals without time limitation. Therefore, gray materials, review articles, commentaries, editorials, and articles presented at seminars and conferences would have been wasted and not included in the review. In addition, this study did not examine all pain tools in non-verbal patients, and only 3 of the pain tools were examined in adult patients. Therefore, the results of the study can be generalized only to adults.
CONCLUSION
Patients hospitalized in ICUs usually suffer from mild to severe pain, and most of them are not able to self-report pain. Thus, behavioral scales are mostly used for pain assessment in mechanically ventilated patients. Besides, vital symptoms are not a reliable index for pain assessment as they can be affected by different factors, such as drugs and diseases. In addition, available data illustrate that CPOT and BPS are superior to NVPS. The ease of use and the team familiarity should be considered when making decisions on the use of pain assessment scales. All members of the treatment team should consider that rapid and effective pain relief plays an important role in stress reduction, prevention of complications, and improvement of post-discharge quality of life. Finally, Healthcare professionals should notice and control pain as a vital symptom.
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
PRISMA guidelines were followed in this study.
FUNDING
None.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflicts of interest.
ACKNOWLEDGEMENTS
Declared none.