All published articles of this journal are available on ScienceDirect.
Multimodal Analgesia Transversus Abdominis Plane Block-Ketorolac Combination being Superior to Paracetamol-Ketorolac as Postoperative Pain Management after Cesarean Section in an Indonesian Hospital
Abstract
Aim:
This study aimed to compare the outcome of multimodal analgesia using transversus abdominis plane block combined with ketorolac and multimodal analgesia oral paracetamol combined with ketorolac in postoperative pain after cesarean section.
Background:
Post-caesarean section pain resulted in prolonged recovery time, inhibited early breastfeeding initiation, and prolonged hospitalization. Multimodal analgesia is an important component of post-cesarean section pain management but has not been established in many Indonesian hospitals.
Methods:
This study was a retrospective, observational analytic study on 46 patients who received low-dose sub-arachnoid block anesthesia. A total of 24 subjects received bilateral transversus abdominis plane block employing ultrasonography-guided lateral approach, with Ropivacaine 0.25% in a total volume of 30cc combined with intravenous ketorolac 30 mg/8 h (Group B). A total of 22 subjects received oral paracetamol 500 mg/6 h combined with intravenous ketorolac 30 mg/8 h (Group A). Numeric Rating Scale (NRS), length of hospitalization, and mobilization time were analyzed using the T-test at a significance level of p<0.05 (confidence interval of 95%).
Results:
The NRS and mean time to start mobilization of patients who received transversus abdominis plane block combined with ketorolac were significantly better than patients who received paracetamol combined with ketorolac (p<0.05). There was no significant difference in the length of hospitalization between the two techniques (p>0.05). Both modalities resulted in improvement in pain intensity over the mild pain range.
Conclusion:
Multimodal analgesia transversus abdominis plane block combined with ketorolac is superior to paracetamol combined with ketorolac for postoperative pain management after cesarean section.
1. INTRODUCTION
In the few decades, cesarean section deliveries have become more common to terminate the pregnancy. Globally, it is estimated that 15% of deliveries are performed by cesarean section. In Europe, 21.1% of deliveries are performed by cesarean section and 32% in the United States [1, 2]. In Indonesia, the cesarean section has increased significantly from the year 2010-2013, growing from 9.8% to 17.6% [3].
Patients potentially experience postoperative pain after undergoing cesarean section. Postoperative pain is caused by surgical trauma and inflammation that promote somatic and visceral pain. Somatic pain in cesarean section arises from noxious stimuli on nociceptors due to skin incisions, whereas visceral pain arises from the incision and uterine contractions. Apart from hormonal changes in pregnancy, psychosocial and emotional factors also play a role in postoperative pain. The mean pain score in the cesarean section was found as 4.7 (moderate pain), higher than spontaneous delivery (3.3 or mild pain) [1, 4]. It is essential to understand the risk factor of chronic postoperative pain development. The postoperative pain causes disruption in the postpartum period, prolonged recovery time, inhibition of early breastfeeding initiation in infants, more extended hospital stays, and even morbidity of the mother [2, 5, 6]. Postoperative pain that is inadequately handled increases the risk of chronic pain up to 2.5 times. The data show that six months after cesarean section, 12.3% of patients experienced persistent pain in the operation area, while 6% of parturients experienced chronic pain one year after the cesarean section [1, 7, 8].
The American Society of Regional Anesthesia recommends some postoperative pain management modalities, including pharmacological therapy (opioid, non-opioid with Non-Steroidal Anti-inflammatory Drugs (NSAIDs) and paracetamol), local anesthesia in the area of the incision, regional anesthesia technique (transversus abdominis plane block), neuraxial anesthetic techniques (epidural, intrathecal opioids), and non-pharmacological therapy (cognitive modalities, transcutaneous electrical nerve stimulation) [9]. Opioids (fentanyl, morphine, meperidine) are the most widely used pharmacological therapies after cesarean section, either intravenous or neuraxial. However, opioid use has many side effects, such as decreased lactation, sedation, respiratory depression, pruritus, nausea, vomiting, constipation, and urinary retention. NSAIDs (ketorolac) play a significant role in visceral pain, but postoperative pain scores persist at 4.14 [10]. Multimodal analgesia may prove to be promising in postoperative pain management as it can exert minimal side effects using opioids and enable a faster recovery period [5]. Multimodal analgesia combines different techniques and medications in order to induce minimum side effects [11, 12].
In Dr. Saiful Anwar General Hospital, Indonesia, cesarean section is mostly done with regional anesthesia subarachnoid block. Post-cesarean section pain management mostly uses multimodal analgesia intravenous ketorolac combined with oral paracetamol. However, there exist no empirical data yet regarding those combinations' outcomes in Dr. Saiful Anwar General Hospital in Indonesia. Our study aims to compare the outcomes of multimodal analgesia ketorolac-paracetamol and transversus abdominis plane block-ketorolac for postoperative pain management after cesarean section.
2. METHODS
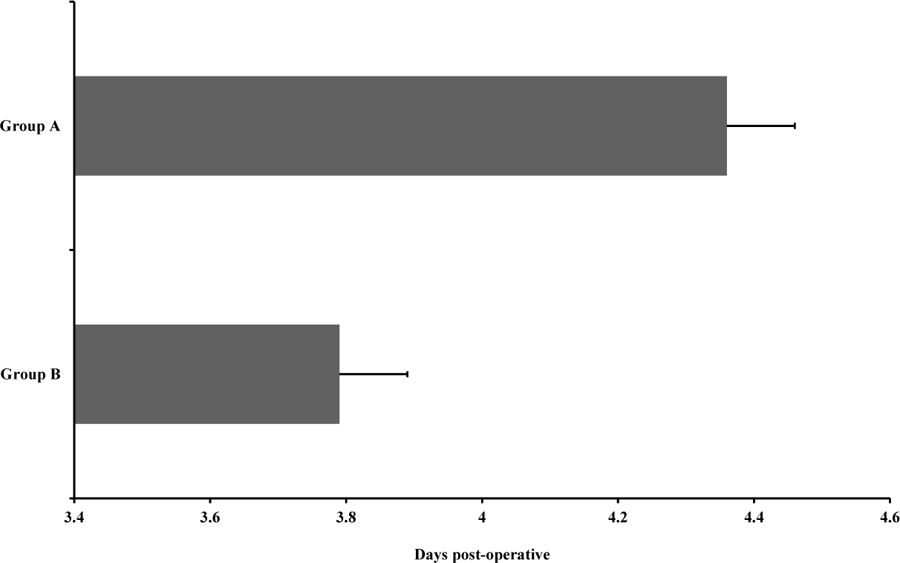
The study was a retrospective analytic observational study conducted in Dr. Saiful Anwar General Hospital, Indonesia, between January 2020-August 2020. The study was approved by the Dr. Saiful Anwar Health Research Ethics Committee (No. 400/221/K.3/302/2020). The study population included parturients who underwent cesarean section. The study subjects were distributed into two groups. Group A received multimodal analgesia intravenous (IV) ketorolac combined with oral paracetamol, while group B received multimodal analgesia transversus abdominis plane block combined with ketorolac. The number of study subjects was calculated based on the following formula proposed by Dahlan [13].
 |
n= the number of the minimum sample
Zα= deviation α=0.05 (1.64)
Zβ= deviation β=0.10 (1.28)
X1-X2= the difference in the minimum mean which is considered significant (1.5)
Sg= standard deviation n1 and n2
S1= standard deviation of the previous study for n1
S2= standard deviation of the previous study for n2
Based on the formula, in each group, the minimum number of subjects was (n) = 19.4. Due to n1= n2, the total number of study subjects was 20 in each group (or 47 in total). The inclusion criteria involved parturients who underwent cesarean section using spinal anesthesia; half of the parturients received transversus abdominis block multimodal analgesia, while the other half received paracetamol orally, ASA status 1, 2, 3. The exclusion criteria included parturients who received general anesthesia, and whose medical data were incomplete.
The subjects were chosen using the randomization technique by the medical data record administrator who did not participate in the study. After randomization, 46 subjects who met the inclusion criteria were selected.
Group A (n=22) received a multimodal analgesia regimen of oral paracetamol 500 mg every 6 hours combined with ketorolac 30 mg (i.v) every 8 hours. Group B (n=24) received multimodal analgesia bilateral transversus abdominis plane block using Ultrasound guidance with Ropivacaine 0.25% in a total volume of 30 cc combined with ketorolac 30 mg (i.v.) every 8 hours. Transversus abdominis plane block is an afferent nerve block technique performed by injecting a local anesthetic regimen into the fascia plane between the transverse abdominis and oblique internal muscles. The study assesses the Numeric Rating Scale (NRS) 22 and 24 hours postoperatively, time of starting mobilization, and the length of hospitalization.
2.1. Statistical Analysis
We used the confidence interval (CI) of 95% and α= 0.05. The data were analyzed using a T-test and employing Statistical Package for Social Sciences (SPSS) (version 18.0, IBM Statistic, United Stated) to analyze the difference in NRS between the two groups (significant if p-value <0.05). Before performing the T-test, all the data were tested for normality and homogeneity. The data not normally distributed (significant at p-value >0.05) were analyzed using the non-parametric Mann-Whitney test (significant at p-value <0.05).
3. RESULTS
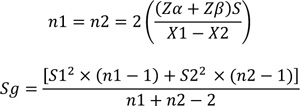
46 patients who underwent cesarean section under spinal anesthesia with different postoperative pain management were selected for the study. The characteristics of the subjects are shown in Table 1. Subjects in both the groups were homogeneous (p> 0.05) (Table 1). Post-operative pain intensity after multimodal analgesia was evaluated based on the subject's NRS (at rest and movement), the subject's ability to start mobilization, and duration of hospitalization. There were significantly different NRS results during rest and movement between group A and group B (p-value <0.05) 12 h and 24 h postoperative (Fig. 1). The NRS at rest and movement of group B was significantly lower than group A.
| Characteristic | Group B (n=24) | Group A (n=22) | p-value |
|---|---|---|---|
| Age (mean) | 30.71 | 29.14 | 0.391 |
| Physical status • ASA 1 • ASA 2 (n) • ASA 3 (n) |
- 16 8 |
- 12 10 |
0.405 |
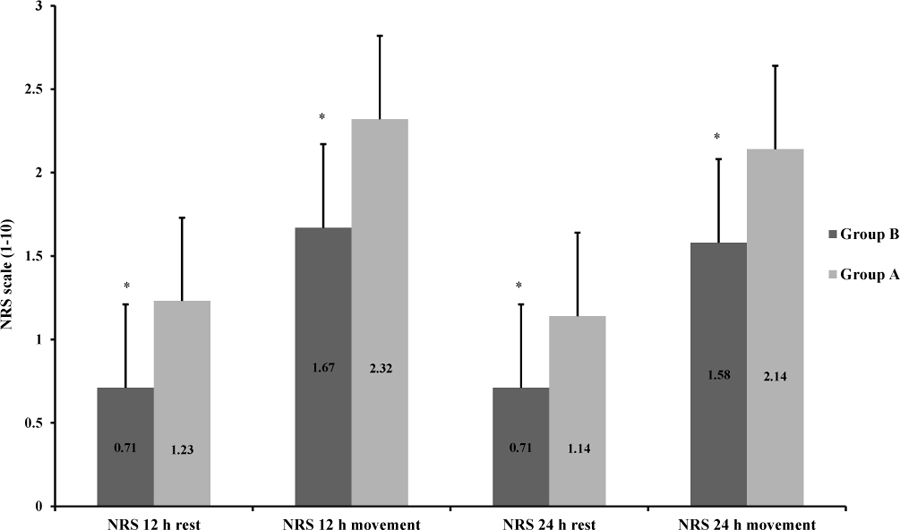
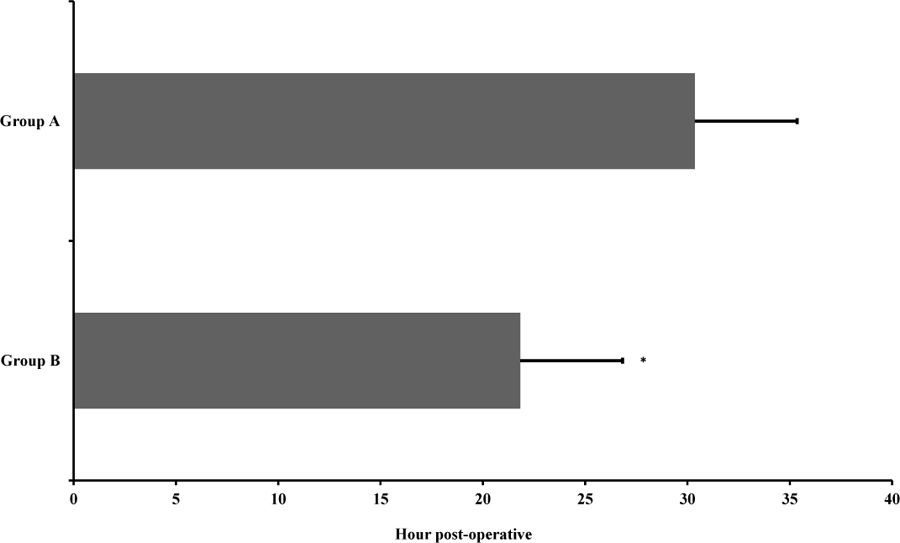
Group B significantly needed a shorter time to start mobilization after the cesarean section than group A (p<0.05). Group B needed 21.83 h postoperative to start mobilization, while group A required 30.36 h to start mobilization (Fig. 2). Subjects in group B exhibited a lower duration of postoperative hospitalization (3.79 days) than group A (4.36 days). However, the statistical test showed no significant difference (p >0.05) (Fig. 3).
4. DISCUSSION
Multimodal transversus analgesia abdominis plane block combined with ketorolac was found to be more effective than the combination of paracetamol and ketorolac. Based on the NRS score in the first 24 h postoperative, the transversus abdominis plane block combined with ketorolac reduced the NRS post-cesarean section. The mean NRS was 4.7 (moderate pain) in the first 24 hours [4]. In this study, the NRS for postoperative 24 hours was 0.71-1.5. The pain intensity ranged from no pain to mild pain.
Multimodal analgesia combination comprising transversus abdominis plane block and ketorolac reduced the dosage of the anesthetic agent and increased the analgesic effect of the analgesic agent. Kasensin et al. state that the use of single ketorolac as analgesia can reduce visceral pain, but the mean NRS score postoperative is 4.14 [10]. This study shows that ketorolac's combination with other modalities increases the effect of ketorolac in reducing the degree of postoperative pain.
Paracetamol can act as an adequate analgesia at a dose of 600-1000 mg every 4-6 hours. At that dose, paracetamol decreased the initial pain intensity by 50% [14]. With the multimodal analgesia technique, the dose can be reduced and the analgesic effect can be increased [15]. This is consistent with our study where paracetamol 500 mg every 6 hours combined with ketorolac reduced the pain intensity from moderate to mild pain post-cesarean section. The mean NRS at rest and movement in the patient who received ketorolac combined with paracetamol was lower than the mean NRS in the cesarean section, which was 4.7 in the first 24 hours. However, the NRS of the patients who received paracetamol combined with ketorolac was still higher than those who received transversus abdominis plane block combined with ketorolac.
The use of a low-dose anesthetic agent is one of the goals of multimodal analgesia. A study by Ng et al. using transversus abdominis plane block for the post-cesarean section with low dose Ropivacaine (0.25%) showed reduced toxicity of local anesthetics. However, the analgesic effect and opioid-sparing effect did not differ with the intermediate (0.375%) or high (0.5%) dose [16]. The use of transversus abdominis plane block for post-cesarean analgesia provides lower pain intensity and reduces the use of opioid in post-cesarean section analgesics [17]. In this study, the combination of transversus abdominis plane block and ketorolac proved to be superior to paracetamol and ketorolac for post-cesarean section analgesia.
The postoperative pain disrupts the postpartum period, prolongs recovery time, inhibits early breastfeeding initiation in infants, and extends the hospital stay [2, 5]. Patients with multimodal analgesia transversus abdominis plane block combined with ketorolac significantly had early mobilization than patients who received multimodal analgesia paracetamol combined with ketorolac. Early mobilization is associated with positive implications, such as faster recovery time, faster initiation of breastfeeding, and shorter hospital stay. Meanwhile, the longer time to start mobilization slow downs the recovery rate, interrupts the bonding between babies and mothers, and increases the length of hospital stay [5, 18].
Patients who received multimodal analgesia transversus abdominis plane block combined with ketorolac significantly had a shorter duration of hospital stay than patients who received multimodal analgesia paracetamol combined with ketorolac. This study supports the findings of previous studies stating that multimodal analgesia provides a shorter hospitalization duration, reduces adverse socioeconomic implications and increases the recovery times [19-21].
The limitation of the study is the minimum number of study subjects. This study is considered a pilot study and further studies need to be conducted involving a more significant number of study subjects.
CONCLUSION
Multimodal analgesia transversus abdominis plane block combined with ketorolac is superior to paracetamol combined with ketorolac as post-cesarean section analgesia.
AUTHORS’ CONTRIBUTION
Isngadi, Djudjuk R. Basuki, Eko Nofiyanto, and Ristiawan M. Laksono contributed equally to conceptualization, literature search, data acquisition, data analysis, manuscript preparation, and manuscript review.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study has been approved by the Dr. Saiful Anwar Health Research Ethics Committee (No. 400/221/K.3/302/2020).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or research committee, and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all the participants.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article are available within the article.
STANDARDS OF REPORTING
STROBE guidelines and methodologies were followed in this study.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


