All published articles of this journal are available on ScienceDirect.
The Management of Complex Regional Pain Syndrome-associated Foot Pain using a Poron Insole, a Sponge Upper Padding, and a Post-operative Shoe: A Case Report
Abstract
Background:
Pain from complex regional pain syndrome (CRPS) is frequently refractory to various treatment methods. Here, we present a case wherein foot pain from CRPS I was managed by applying an insole made from poron (a soft polyurethane foam and highly absorbent material for shock reduction), a sponge upper padding, and a post-operative shoe.
Case Presentation:
A 47-year-old female patient with CRPS I on her left foot complained of pain for a few months, which was aggravated while standing and walking [numeric rating scale (NRS): 8]. She had a history of a linear fracture in the distal portion of the left 1st metatarsal bone 5 months ago, and the pain from CRPS started 2 months after the fracture. We believed that the aggravated pain during standing and walking was allodynia. We utilized a poron insole, a sponge upper padding, and a post-operative shoe to reduce the pressure and friction loading on her left foot. 1 month after this intervention, the patients’ pain during standing and walking was found to have reduced from NRS 8 to NRS 3. At her 3- and 6-month follow-ups, the degree of pain was sustained at NRS 3.
Conclusion:
We believe that the reduction of allodynia using materials, which can absorb mechanical pressure and friction of the foot, can help manage pain from CRPS.
1. INTRODUCTION
Complex regional pain syndrome (CRPS) is a chronic severe pain condition that involves vasomotor changes, including edema, changes in skin color and temperature, increased sensitivity to tactile stimulation (allodynia), and limitation in the range of motion [1]. Although its etiology is not clearly understood, CRPS is known to occur after damage to the peripheral and central nervous systems and also can develop after direct trauma to the arm or leg [1]. CRPS is divided into two types depending on the presence or absence of identifiable peripheral nerve damage: CRPS I occurs after an injury or disease that does not directly damage nerves in the affected limb, and CRPS II follows a distinct nerve injury [1, 2].
There is no gold standard for the treatment of CRPS [3]. Various oral medications, such as nonsteroidal anti-inflammatory drugs, anti-convulsants, analgesics, and antidepressants, are being used to alleviate pain [4]. Also, short-term oral prednisolone therapy, sympathetic blocks with local anesthetics, and psychiatric management therapies have been used [4]. However, many cases of CPRS are refractory to these treatment methods.
Allodynia is one of the most common clinical complaints of CRPS [5]. Patients with CRPS are extremely sensitive to touch and/or physical pressure [5]. Therefore, when CRPS occurs in the foot, pain is aggravated during standing or walking, which leads to difficulty in ambulating [5, 6]. In 2008, Actis et al. reported that in diabetic patients with foot ulcers, using a soft topical plug such as poron is a good strategy to reduce the maximum pressure on the foot [7]. In 2021, Hoang et al. stated that the use of semi-rigid materials, such as EVA, poron, and polypropylene in foot orthoses could relieve foot pain by dispersing the pressure on the foot [8]. In addition, the width of the shoe contributes to the pathology of the foot, which is evident from previous studies that have shown that people who wear wide shoes have less pain in their feet than people who wear narrow shoes [9]. Therefore, we considered that the reduction of pressure on the foot using soft insoles and wide-width shoes could help relieve pain following CRPS. However, the utilization of these insoles or shoes for managing foot pain induced by CRPS has not been reported yet.
In this study, we presented a case where foot pain from CRPS I was managed by applying insoles made from poron (a soft polyurethane foam and highly absorbent material for shock reduction), a sponge upper padding, and a post-operative shoe.
2. CASE PRESENTATION
The study protocol was approved by the Institutional Review Board of Yeungnam University Hospital, and written consent was waived because this study was an anonymized case report. A 47-year-old woman visited the physical medicine & rehabilitation department complaining of continuous burning and sharp left foot pain that had been ongoing for 3 months [numeric rating scale (NRS): 3], and was aggravated while standing and ambulating [numeric rating scale (NRS): 8]. Five months before the visit, she had a traffic accident that involved the wheel of a car passing over her left foot. A linear fracture in the distal portion of the left 1st metatarsal bone was diagnosed on magnetic resonance imaging (MRI). The fracture was conservatively treated, and it healed.
However, she had persistent pain afterward, which was disproportionate to any inciting event. Additionally, during physical examination, she was found to have hyperesthesia and allodynia of her entire left foot. Edema, warmth, and reddish skin color were observed in the left foot. In a nerve conduction study, no abnormal findings were noted. Based on the CRPS criteria proposed by the Budapest consensus group1, we diagnosed her with CRPS I. We administered oral medications, including 16 mg of oral prednisolone, 150 mg/1300 mg of tramadol/acetaminophen, and 10 mg of buprenorphine, but no reduction in pain was observed.
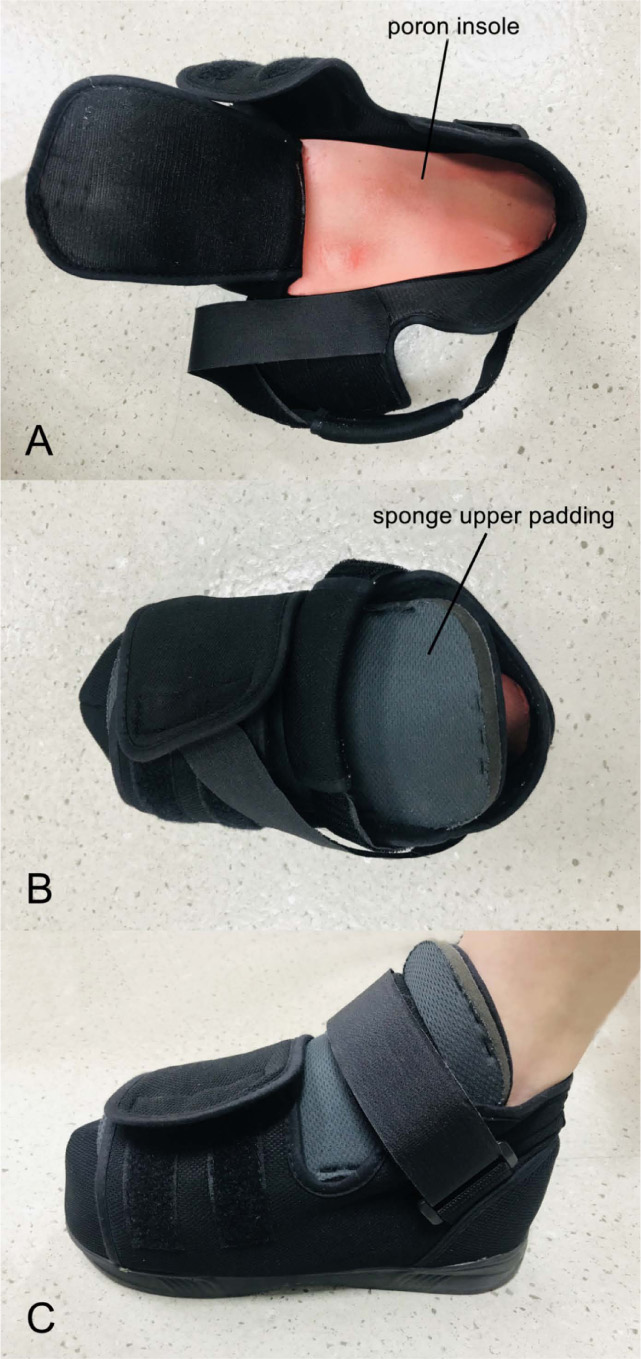
We believed that the aggravated pain during standing and ambulation was allodynia. Therefore, to reduce the allodynia from touch or physical pressure, we applied a poron insole (thickness: 12.8 mm) and a sponge upper padding (thickness: 1 cm, size: 8 x 17 x 1 cm3) on the dorsum of the left foot (Fig. 1). Also, to prevent compression on the foot, we utilized a post-operative shoe (Fig. 1). No other device for pain management was used.
At the 1-month follow-up after applying the poron insole, sponge upper padding, and post-operative shoe, the patient’s pain during standing and ambulating was reduced from NRS 8 to NRS 3, although her resting pain had not decreased. When the patient was not wearing the post-operative shoe with the poron insole and sponge upper padding, no reduction in pain was noted. At the 3- and 6-month follow-ups, the degree of pain was sustained at NRS 3.
3. DISCUSSION
We successfully controlled allodynia using a poron insole, a sponge upper padding, and a post-operative shoe on a patient with CRPS. Poron is a soft and resilient polyurethane foam that effectively absorbs mechanical stress [10]. The poron insole is used generally to prevent diabetic ulcers and to manage pain caused by various foot disorders, such as plantar fasciitis, plantar fascial fibromatosis, and metatarsalgia [10]. For our patient, the poron insole reduced mechanical pressure on the affected foot, alleviating pain from allodynia following CRPS. Additionally, the sponge upper padding was used to reduce the mechanical pressure and friction between the shoe and the dorsum of the foot, which seemed to have attributed to pain reduction. Lastly, we applied the postoperative shoe, which has a Velcro strap that can be tightened or loosened to adjust the width and size of the shoe. Therefore, with the postoperative shoe, it is easy to insert the sponge upper padding between the dorsum of the foot and the shoe. Also, the postoperative shoe is loose and light; thus, it reduces the compression on the foot and helps manage the pain due to allodynia.
CONCLUSION
Many previous studies have suggested several treatment strategies for CRPS, such as oral medications, physical therapies (progressive weight-bearing, active and passive range of motion, and transcutaneous electrical nerve stimulation), and procedures (sympathetic nerve block and spinal cord stimulation) [1, 3, 4]. However, taking measures for the reduction of mechanical pressure on the affected extremity to alleviate pain from allodynia has not been attempted. In this study, we demonstrated that reduction of the pressure or friction loaded on the affected extremity can help manage pain from CRPS.
We utilized a poron insole, sponge upper padding, and post-operative shoe for a patient with CRPS of the left foot, which reduced the patient’s pain by more than 50%. Our study is the first to apply a soft insole and sponge to reduce the pressure on the foot and alleviate pain from allodynia in a patient with CPRS. We believe that our treatment method would be a beneficial option for clinicians aimed at pain management resulting from CRPS. Our study is limited in that it is a case report. Therefore, further studies involving a larger number of subjects are required to confirm this finding more broadly.
LIST OF ABBREVIATIONS
| CRPS | = Complex Regional Pain Syndrome |
| NRS | = Numeric Rating Scale |
AUTHORS’ CONTRIBUTIONS
YJC and MCC interpreted the patient data and drafted the manuscript; YJC, MB, ISP, and MCC reviewed the literature and revised the manuscript; YJC, MB, ISP, and MCC read and approved the final manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study protocol was approved by the Institutional Review Board of Yeungnam University Hospital, (protocol number: YUMC 2021-04-055, approval date: May 7, 2021).
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. The reported experiments were in accordance with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written consent was waived because this study was an anonymized case report.
STANDARD OF REPORTING
CARE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
All data generated or analyzed during this study are included in this published article.
FUNDING
The present study was supported by a National Research Foundation of Korea grant funded by the Korean government (grant no. NRF-2019M3E5D1A02069399).
CONFLICT OF INTEREST
The authors report no conflicts of interest related to this work.
ACKNOWLEDGEMENTS
Declared none.


