All published articles of this journal are available on ScienceDirect.
Things to know about Sacroiliac Joint Pain
Abstract
Background
Sacroiliac Joint dysfunction is a significant pain generator (>25%) in Lower Back Pain patients; however, differential diagnosis and treatment in these patients can be challenging for pain physicians. Understanding its complex anatomy, function, and possible primary and secondary pain etiologies is essential to formulate appropriate diagnostic workup and treatment options for SI joint disorders.
Objective
To report a concise narrative review of the Sacroiliac Joint anatomy, function, and injury mechanisms, along with an overview of its painful dysfunction diagnosis workup and potential treatments.
Methods
A concise summary of the current literature relevant to Sacroiliac Joint dysfunction, putting previous research and findings in context and presenting recent developments in a critical and focused manner.
Results and Conclusion
Sacroiliac Joint dysfunction diagnosis is challenging given its complex anatomy, physiology, and variable mechanisms of injury and pain presentation features. According to the underlying etiopathogenesis, SIJ dysfunction chronic pain may be secondary or primary (arising or not from an underlying classified disease, respectively). The clinical implications of this review are (a) for the diagnosis workup, a combination of history, physical examination, specific provocative tests, articular and periarticular block, and appropriate imaging is imperative; (b) treatment may include conservative management, therapeutic blocks (intra- and periarticular) with local anesthetics and corticosteroids, neuro ablation (Crio or Radio Frequency techniques), and surgery for patients unresponsive to therapies.
1. INTRODUCTION
Dysfunction or injury at the Sacroiliac Joint (SIJ) anatomical area is a significant pain generator in Lower Back Pain (LBP) patients, affecting 10 to 62% of these patients, with a point prevalence of roughly 25% [1-4]. The SIJ's peculiar anatomy (bones, muscles, ligaments, and innervation), physiology, and possible injury or dys- function mechanisms may yield various pain patho- physiology processes and correlated symptoms. Thus, SIJ pain differential diagnosis and treatment in LBP patients can be challenging. Clinical evaluation should combine patient history, physical examination, and radiological studies, while treatments should follow a multimodal “step-by-step” approach.
The new International Classification of Disease (ICD-11) introduces the concept of chronic primary (MG30.02) and secondary (MG30.3) musculoskeletal pain [5]. Accordingly, SIJ chronic pain classification can also be primary or secondary. Chronic primary SIJ pain is a condition not better accounted for by a classified disease. Chronic secondary SIJ pain arises from an underlying classified disease. In the latter, local or systemic pathologies or deep somatic lesions promote persistent nociception triggering within the SIJ anatomical structures. Underlying pathologies may be inflammation, structural changes of various origins, or biomechanical consequences of nervous system diseases [6].
We sought to gather literature and prominent essential knowledge concerning SIJ pain concisely and practically for a rapid and comprehensive overview.
2. ANATOMY
The SIJ is the largest axial joint in the body, with an average surface area of 17.5 cm2 [7]. The sacral and the iliac bones form the SIJ's articular surfaces, delimiting, in the adult, an auricular-shaped (also described as C- or L-shaped) joint. The iliac articular surface is convex and fibrocartilaginous, while the sacral surface is concave and covered by abundant hyaline cartilage. Both iliac and sacral articular surfaces are irregular, with multiple adapting ridges and depressions, yielding a high friction coefficient that reduces mobility and increases stability [8, 9]. The SIJ’s capsule consists of both continuation and extension to the local ligamentous framework. Interestingly, the capsule’s posterior aspect, made of numerous bands of interosseous ligaments, is caudally discontinued, allowing a close relationship between the SIJ and nearby neural elements.
An evolving understanding of the SIJ mobility features gave rise, over time, to different SIJ anatomical definitions. These definitions included amphiarthrosis, a mixed and minimally movable joint in which “articulating surfaces are covered with fibro-cartilage, partially lined by a synovial membrane, and connected by external ligaments [10];” an intermediate joint between a synarthrosis (immovable bone elements united by a fibrous apparatus) and a diarthrosis (freely movable joint) [11]; and Diarthro-amphiarthrosis; a combination of a freely movable ventral aspect and an ossified immovable dorsal aspect [12].
Finally, Cohen reported that only the anterior third of the sacrum/ilium interface is an authentic synovial joint covered by hyaline cartilage that provides a gliding surface between the bones [2]. The rest of the joint comprises intricate fibrocartilaginous ligament connections, enhancing the SIJs’ stability. The posterior capsule of the joint is absent or rudimentary.
2.1. Muscles
Over 40 muscles surround the SIJ. These muscles essentially promote the SIJ stability and function rather than its movement. It is the SIJ ligaments' tension that specifically guarantees its movement. Muscle groups involved with the SIJ are:
- Back muscles (e.g., erector spinae, quadratus lumborum, and multifidus lumborum).
- Hip muscles (e.g., iliopsoas).
- Core muscles (e.g., rectus abdominis).
- Buttock muscles (e.g., gluteus maximus and piriformis).
- Thigh muscles (e.g., biceps femoris).
Table 1 describes SIJ’s main muscles and their SIJ-related function. These muscles may compress the SIJ, tense its ligaments, and contribute to the SIJ nutation and counternutation movements [13-15].
2.2. Ligaments
Some strong ligaments stabilize the SIJ to enable its physiological function [13, 14, 16-18]. The main ligaments of the joint are the anterior and posterior sacroiliac ligaments. Accessory ligaments like the sacrotuberous and sacrospinous add stability to the SIJ. Table 2 describes these ligaments' anatomical and functional features. Fig. (1) is a semi-schematic representation of the main SIJ posterior-aspect ligaments and their anatomical insertions.
2.3. Innervation
The innervation of the SIJ is still not fully described. Nerve fiber endings have been described within the joint capsule and annexing ligaments. Authors agree that the lateral branches of L4-S3 dorsal rami supply the posterior SIJ, while L2-S2 innervates the anterior aspect of the joint [1, 2]. Like other synovial joints, the SIJ periarticular tissues contain mechanoreceptors and nociceptors. These receptors may relay somatosensory information and contribute to the SIJ area pain pathophysiology [19].
3. FUNCTION AND BIOMECHANICS
The SIJ is a highly specialized joint that enables stable and flexible support to the upper body [1]. SIJs are essential for transferring loads between the spine and the legs. The sacrum, pelvis, and spine connect to the limbs and trunk through muscular, fascial, and ligamentous interconnections. Physiologically, the trunk and lower limbs interact through the pelvic girdle, transferring forces and motions bi-directionally. In this interaction, SIJs act as stress relievers and prevent an otherwise solid bony pelvic ring from being subject to excessive shear forces and, thus, lesions or fractures [20, 21]. The SIJ, therefore, acts as a self-accommodating interface of loads between the upper body and the legs. In this context, the SIJ absorbs, diverts, and mitigates the forces generated by any body movement that might affect the pelvis and the spine. Any failure in the functions mentioned earlier may cause SIJ dysfunction and pain.
| Muscle | Major Function | SIJ related Function | Notes |
|---|---|---|---|
| Gluteus maximus | Hip extensor | SIJ compression | Muscle fibers assemble with thoracolumbar fascia and sacrotuberous ligament. |
| Biceps femoris long head | Knee flexion and hip extension. | Overlapping the ischial tuberosity, it increases tension upon the sacrotuberous ligament. |
Muscle fibers assemble with the sacrotuberous ligament. |
| Piriformis | Femur external rotation | SIJ compression | With iliac and sacral origin, it crosses the SIJ perpendicularly. |
| Latissimus dorsi | Participates in lifting the pelvis (aside upper body movements) | Increase compressive forces over the SIJ. | Starting from the lower six thoracic spinous processes and through the thoracolumbar fascia, it inserts on the iliac crest and blends with the contralateral gluteus muscles. |
| Multifidus | Static and dynamic spinal stability | Contributes to nutation. | It is primarily developed in the lumbar area and expands over the entire vertebral column. Its origin is the sacrum back surface, PSIS, lumbar vertebrae mammillary processes, and thoracic vertebrae transverse processes. It inserts at the spinous process of all vertebrae from L5 to T8, 2-4 levels above the origin. |
| Erector spinae | Extend and laterally flex the spine. | Contributes to nutation. | Its Iliocostalis lumborum portion arises from the Iliac crest. It inserts at the L1-L4 lumbar transverse processes, 4 to 12 ribs angle, and thoracolumbar fascia. |
| Transverse abdominal muscle | Primary spinal stabilization muscle. | Decreases the SIJ’s laxity; active in both nutation (primarily) and counternutation. | It arises from the inguinal ligament lateral third and adjacent iliac fascia, iliac crest anterior two-thirds, thoracolumbar fascia, and the inner surface of lower 6 costal cartilage and ribs. Insertion includes the linea alba, internal abdominal oblique muscle aponeurosis, pubic crest, and pubis pectinal line. |
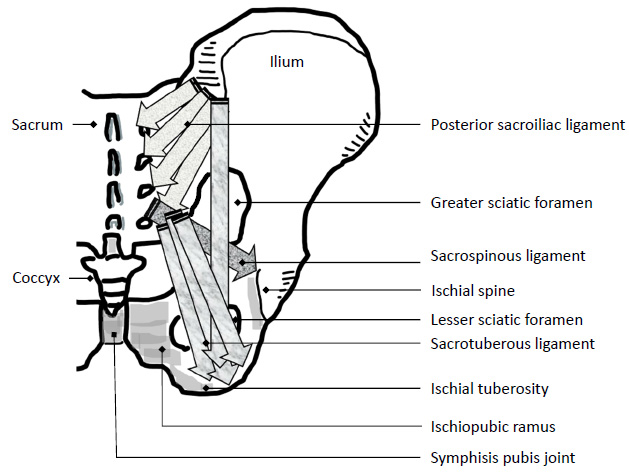
Semi-schematic illustration of the SIJ posterior aspect ligaments.
| Ligament | Anatomical Insertions/features | Function/notes |
|---|---|---|
| Anterior sacroiliac ligament | An anterior-inferior thin thickening of the SIJ capsule. It extends from the ilium’s ala, anterior to the auricular surface, to the sacrum pelvic surface. | Most vulnerable to injury and a common source of pain. |
| Interosseous sacroiliac ligament | A robust short band between the sacrum and ilium that attaches to their tuberosities behind the auricular surfaces. | A major connection between the sacrum and the ilium prevents anterior and inferior movement of the sacrum. |
| Posterior (dorsal) sacroiliac ligament | Between the posterior-superior iliac spine and the iliac crest to the third and fourth segments of the sacrum. | Limits sacral counternutation |
| Sacrotuberous ligament* | Three bands: one band originates between the posterior superior and inferior iliac spines and mingles with the posterior sacroiliac ligament; another one arises on the sacrum lateral side below the auricular surface, and the third on the coccyx upper lateral side. The three bands converge inferiorly, forming a triangular shape, and are inserted on the lower margin of the ischial ramus. | Limits sacral nutation |
| Sacrospinous ligament* | It originates on the ischial spine and attaches to the lateral lower sacral and upper coccygeal segments, anterior to the sacrotuberous ligament. | Limits sacral nutation during weight-bearing and gait. |
The SIJ movements are generally described as nutation (forward dislocation: the sacrum shows anterior-inferior movement while the coccyx moves posteriorly) and counternutation (backward dislocation: the sacrum shows posterior-superior movement while the coccyx moves anteriorly).
These movements involve a few degrees of rotation around the transverse axis of S2 and slight translation [3]. Fig. (2) is a semi-schematic illustration of the SIJ's nutation and counternutation movements; red and green dashed arrows indicate sacral and ilium movement directions.
Form and force closures contribute to the SIJ stability. Form closure derives from the stable close fitting of the SIJ articular surfaces. However, to enable mobility and face dynamic vertical load increase and shearing forces, perpendicular compression force (i.e., force closure generated by muscles and ligaments), along with nutation movement, adapts the SIJ to overcome any dynamic and gravity forces [9].
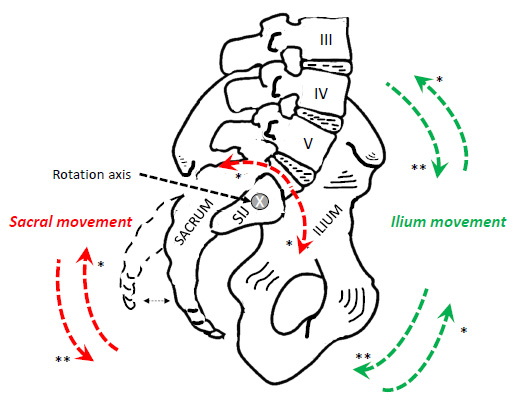
Semi-schematic illustration of the SIJ's nutation and counternutation movements.
4. MECHANISM OF INJURY
The anatomical characteristics of the SIJ make it vulnerable to various modes of stress and injury. The bony anatomy is highly variable in size, shape, and contour among individuals [22]; for example, females have a narrower sacral angulation compared with males, a shorter posterior sagittal diameter of the pelvic outlet, and a narrower sacrum.
Moreover, the shape of the joint changes markedly from infancy to adulthood [23]. These changes lead to a degenerative process that restricts SIJ motion as its capsule becomes more collagenous and fibrous ankylosis occurs. By the eighth decade of life, erosions and plaques are inevitable. Pathological changes such as synovial disruption, ligament tension, hyper- or hypo-mobility, fractures, inflammatory processes, and soft tissue injury can lead to SIJ pain.
Accordingly, causes for SIJ pain may arise from intra-articular and extra-articular components or both. In addition, risk factors for SIJ pain include scoliosis, leg length discrepancy, prolonged or repetitive exercise, pregnancy (due to weight gain, lordosis, and hormone-induced ligamental laxity), osteoarthritis, and autoimmune inflammatory diseases such as spondyloarthropathy (both seronegative or HLAB27-positive) [24-28]. Traumatic incidents like direct falling on the buttocks, vehicle accidents involving, directly or indirectly, the pelvis and past lumbar spine surgery may contribute to SIJ dysfunction.
5. PRESENTATION AND DIAGNOSIS
The variable clinical presentation renders SIJ dysfunction diagnosis in LBP patients challenging. Patients may report pain from multiple sites, such as the piriformis region, the thoracolumbar fascia, lumbar disks or facets, lumbar muscles, limbs, and referred pain. Thus, SIJ-related pain may be localized at the Posterior Superior Iliac Spine (PSIS) area and referred to other sites. Fig. (3) is a representation of the most typical SIJ pain referral sites: the lower back, buttocks, and radiation extended to the upper leg, hip, and groin region. Table 3 reports SIJ pain features of localization, intensity, quality, and aggravating factors [29-36]. Causes for the SIJ pain presentation variability are the area peculiar innervation, sclerotomal pain referral, adjacent structures irritation, and the joint’s variable injury localizations [34]. Differential diagnoses of SIJ dysfunction include discogenic and facet joint pains and myofascial and piriformis pain syndromes.
Hence, the authors recommend a patient-centered approach to evaluate an SIJ painful dysfunction.
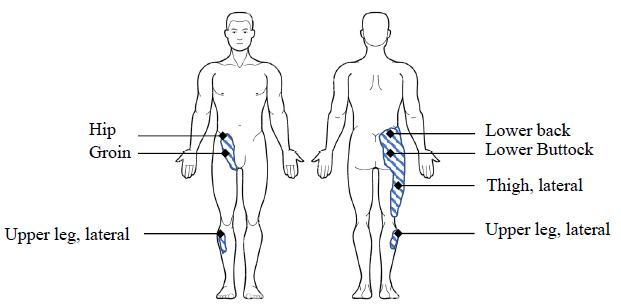
Typical SIJ pain referral sites.
| Localization | o Localized and/or referred pain. o Area of 3 x 10 cm inferior to the PSIS and always beyond the L5 spinous process. o Frequent presentation pain areas: lower back, buttocks (94%), lower lumbar area (72%), lower extremity (50%), hip, leg, upper lateral aspect, and groin (14%). |
| Intensity/Quality | o From dull/achy to sharp/stabbing. o Spasms of local muscles. o Numbness/radicular symptoms. o Allodynia and hyperalgesia are in the area between the SIJ line and the ipsilateral hip, as well as the greater trochanter. |
| Aggravating factors | o Physical activity, sustained positions, sitting, bending, climbing, rising, and sexual intercourse. |
5.1. History and Physical Examination
SIJ pain diagnosis includes a thorough patient clinical history and physical examination. The patient's clinical history aims to uncover possible injury mechanisms and aggravating factors and exclude secondary SIJ disease [1]. Physical examination includes evaluating any possible deformity or leg-length asymmetry and observing daily movements, such as ambulation, sitting, and transitioning to standing. A series of provocative tests to stress the joint and evoke or enhance pain finalize the exam [1, 4]. Table 4 reports the known SIJ provocative tests; it details the patient and examiner's position and actions to accomplish the test and the expected results. The most common SIJ provocative tests include SIJ distraction and compression, FABER (hip Flexion, Abduction, and External Rotation), Gaenslen, and the Thigh Thrust tests. The literature suggests that positive results for three out of the latter tests indicate SIJ dysfunction [38]. Note that positive Thigh Thrust or the SIJ compression test should be among the three positive tests. Other less commonly used SIJ diagnostic tests include the passive straight leg raising, pubic symphysis test, and rectal examination. Finally, the International Association for the Study of Pain (IASP) proposed diagnostic criteria for SIJ dysfunction [6, 39]. These criteria are pain in the area of the SIJ (Table 2), SIJ provocative tests reproduce the patient's pain (Table 3), and selective block of the SIJ with local anesthetic should relieve the patient's pain [1, 4].
| Test | Significance | Patient Position and Actions | Examiner Position and Actions | Positive/expected Result/s |
|---|---|---|---|---|
| Compression test (version 1) * | Eliciting SIJ tenderness. | Lateral position on the affected side. | Applies pressure on one pelvic margin in the direction of the other. | Pain elicited along the SIJ. |
| Compression test at SIJ (version 2) * | Eliciting SIJ tenderness. | Prone. | Places a palm over the SIJ or on the sacrum and applies vertical pressure downward. | Pain/discomfort elicited along the SIJ. |
| Distraction test (version 1) * | Eliciting SIJ tenderness. | Supine position. | Alternately presses each anterior superior iliac spine in a posterolateral direction. | Pain elicited along the SIJ or movement is asymmetrical. |
| Distraction test (version 2) * | Extensile forces are applied onto the anterior part of the SIJ. | Supine, with forearms under the lower back to preserve lordosis and to uphold the lumbar spine. The knees are supported with a pillow. |
With straight elbows and crossed arms, the hands are placed on the anterior and medial portions of both ASIS. Slow and steady force is applied in latero-dorsal direction while leaning down towards the patient. |
Pain elicited along the SI joint. |
| FABER test (hip Flexion, Abduction, and External Rotation, or Patrick’s test) * | Eliciting SIJ tenderness. | Supine, one heel is placed on the opposite knee and the elevated leg is guided toward the examining table. | Gently abducts the elevated leg towards the examining table. | Pain elicited along the SIJ. Trochanteric pain may arise from the stressed hip joint. |
| Fade test | Eliciting SIJ tenderness. | Supine position, the hip is flexed and abducted to midline. | Applies pressure to the long axis of the femur to push the ileum posterior. | Pain elicited |
| Fortin finger test | Pain site localization. | Upright position, showing the back to the examiner; pointing, with one (index) finger, his/her pain area. | Behind the patient inviting him/her to point, with one (index) finger, the pain area. | Patient indicates pain area within 1 cm infero-medially to the PSIS. |
| Gaenslen test * | Forcing the SIJ through maximal range of motion | Supine, hip and knee maximally flexed toward the trunk, and the opposite leg is extended down and off the examining table. | Instructs the patient to the test’s position. | Pain elicited along the SI joint. Trochanteric pain may arise from the stressed hip joint. |
| One-legged stork (Gillet) test | SIJ alignment and mobility | Upright position; flexes the palpated hip to 90°. | Behind the patient, placing his/her thumbs on one PSIS and the sacrum at S2. | The examiner’s thumb moves upward instead of infero-medially, |
| Piedallu or seated flexion test | SIJ alignment and mobility | Patient seated; flexing forward the trunk. | Behind the patient, placing his/her thumbs just below each PSIS. | asymmetry of motion. (i.e., upward motion on the involved side.) |
| Thigh Thrust * | Antero-posterior shear stress application onto the SIJ. | Supine, with the hip of the examined side flexed to 90 degrees | Standing at the same side of the examined SIJ; the right hand is placed on the opposite ASIS to stabilize the pelvis; exerts increasing pressure on the femur axis combining left hand and thorax. | Pain elicited along the SI joint. |
| Van Durson standing flexion test | Assessing SIJ misalignment or abnormal movements. | Upright position; flexing neck and upper thoracic spine forward without bending the knees. | Behind the patient, placing his/her thumbs just below each PSIS. | Asymmetrical PSIS motion (i.e., upward motion of the involved side) |
5.2. Imaging
Imaging of the SIJ is often performed in the early evaluation phase. Such studies aim at identifying pathologies such as fractures, tumors, or local changes related to inflammation and infection. Nonetheless, imaging studies are inaccurate and have variable sensitivity and specificity; their value in the SIJ pain diagnosis has been questioned [4, 40, 41]. Radiological imaging may include plain X-rays (lumbosacral spine, anteroposterior and lateral views; pelvis, anteroposterior view) with low sensitivity and high specificity; plain CT (for bone pathologies but not for local inflammation), MRI (high sensitivity in early sacroiliitis, and follow-up of spondyloarthropathy); single-photon emission computed tomography (SPECT) and positron emission tomography (PET) scanning are of low sensitivity and high specificity; and, US for ligamentous pathology. Finally, imaging in combination with provocative maneuvers may identify patients who might benefit from further evaluation.
5.3. Electroneurography and Electromyography
For LBP patients who report positive or negative neurologic symptoms and signs, differential diagnosis may benefit from electroneurography and electromyography (EMG). The latter may “detect neurogenic changes and denervation, provide physiological significance to anatomic lesions found in imaging studies, and distinguish between radiculopathy, peripheral mononeuropathy, peripheral polyneuropathy, and other lower motor neuron processes” [42].
5.4. Diagnostic Blocks
The literature recommends SIJ intraarticular (with or without periarticular, see below) local anesthetic injection to confirm SIJ dysfunction diagnosis; a 75% reduction of pre-injection pain score is considered a positive test [1, 4, 39, 40, 43]. In the literature, image-guided injection of a local anesthetic is the gold standard for diagnosing SIJ dysfunction [39, 44, 45].
6. TREATMENT
A tailored approach should be the standard of care. Management includes treatments aiming at pain relief and those seeking to manage the underlying cause of SIJ dysfunction [2]. Treatment options include conservative medical management, physical therapy, mini-invasive interventions such as articular injections, nerve blocks and ablations, and surgical SIJ stabilization or fusion.
6.1. Psychosocial Issues
Psychosocial factors can influence chronic SIJ pain development and response to treatment. Common psychiatric diseases that may impact chronic SIJ pain are depression, anxiety, and substance abuse [46, 47]. Social factors, such as return-to-work issues, inadequate coping mechanisms, attitudes, beliefs, and distorted expectations, can impact the prognosis of LBP and SIJ pain [1].
6.2. Conservative Management
SIJ dysfunction management may include three clinical phases: acute (up to 7 days), recovery (8 weeks), and maintenance.
Correctable etiologies and aggravating factors should be identified and treated in the acute first phase. Interventions may include using shoe inserts for leg length discrepancy, pelvic belts for pregnant women to limit the SIJ rotation and motion, and specific pharmacological treatments of the underlying diseases (e.g., inflammatory arthritis and bowel diseases, rheumatoid disease, ankylosing spondylitis, and Reiter’s syndrome) [2, 43, 48].
A multidisciplinary approach is mandatory, consi- dering, for example, the involvement of a rheumatologist. Rest, cold applications, and gentle mobilization with heat may be helpful in the acute phase. Analgesics should be prescribed with caution involving pain specialists. As for nociceptive chronic LBP, muscle relaxants and NSAIDs may be effective for the myofascial and inflammatory components of SIJ pain [49]. Prescription of more potent analgesics or opioids should be guided by the WHO analgesic ladder and tailored to the patient's needs and clinical features [50].
In the recovery phase, physical therapy includes stretching, strengthening, and stabilizing the pelvic floor, gluteal and abdominal muscles and correcting gait and postural abnormalities [51]. Such interventions may proceed through the maintenance phase.
6.3. Articular and Peri-articular Injections
Among non-surgical procedures for SIJ pain, there is little solid evidence for intraarticular injections of corticosteroids and local anesthetics [52, 53]. These injections may have diagnostic and therapeutic functions [54]. The authors agree that corticosteroid injections should be limited to three in six months and four in one year [43, 51].
The literature reports two types of SIJ injections: the intra-articular and the periarticular [55-57]. Intra-articular injections aim at the injectate delivery into the SIJ, while periarticular injections target the SIJ surrounding anatomical structures. Murakami et al. reported that the periarticular SIJ injection was more effective and easier to perform than the intra-articular one. However, their study showed no significant difference between the two procedures. As such, the authors concluded that the peri-articular injection should be performed first, followed by an intra-articular one in case of the former failure [55].
SIJ blocks were reported to be delivered both without imaging guidance, using palpable landmarks only, or to ensure accuracy, with imaging guidance techniques (fluoroscopy, Computed tomography (CT), MRI, or Ultrasound (US) methods [38, 40, 58-61]. In the literature, CT provides better guidance accuracy than fluoroscopy for SIJ injections; the latter is more accurate than the US [62]. However, the burden of considerable costs and health risk issues with some imaging methods (e.g., fluoroscopy and CT) should be carefully considered. US-guided SIJ injections, both accurate and safe, are gaining ample consensus.
Regardless of the imaging method used, the patient’s pain level should be assessed using a 0 to 10 Numerical Rating Scale (NRS) prior to the block. This assessment is particularly essential for diagnostic blocks.
The injectate is usually a mixture of local anesthetic agents of rapid and long duration (e.g., Xylocaine, Marcaine, or Bupivacaine) and eventually corticosteroids (e.g., Metilprednisolone 40 to 80 mg). The total volume injected should be roughly 2 ml, as larger volumes may leak through the SIJ capsule to the adjacent neural structures and give a false-positive result.
Two to four hours after the block, the NRS should reassess the patient’s pain and a reduction of at least 75% from the pre-block pain level is considered diagnostic [1, 4].
6.4. Radiofrequency Denervation Procedures
The percutaneous Radiofrequency Denervation Tech- niques (RDT) are used to disrupt SIJ’s sensory innervation to achieve lasting pain relief. At the moment, there is limited evidence to show the efficacy of RDT. One major issue of the percutaneous RDT is the impossibility of denervating the anterior neural structures of the SIJ, given the complex neuroanatomy of the SIJ itself [43, 63, 64]. RDT may include Conventional, Bipolar, Cooled, Pulsed, and Strip Lesions (i.e., continuous strip lesions from L5 to S4 dorsal rami such as with Guide block or Simplicity probe) all, however, requiring more high-quality and large-scale randomized controlled trials to prove long-term efficacy [65]. A recent systematic review concluded that anatomically validated sacral lateral branch radio- frequency neurotomy may improve SIJ dysfunction and pain [66].
6.5. Prolotherapy
Prolotherapy (i.e., Proliferative Therapy) may also be used for SIJ pain. The rationale for this approach lies in the central role of ligaments and other soft tissue pathologies in developing LBP and SIJ pain. This procedure uses agents like phenol or a glucose-based solution injected at the base of the ligamentous complex to promote an inflammatory response. The latter may cause fibroblastic migration and increased ligamentous laxity, reducing the SIJ area's pain [43, 67, 68].
6.6. Surgical Interventions
Surgical arthrodesis can be considered for patients whose SIJ pathology and pain are unresponsive to less invasive treatments. With this approach, the SIJ’s space is obliterated, and pain caused by the SIJ motion is reduced. Both open anterior and posterior approaches are possible. In the literature, there is an increasing trend toward minimally invasive forms of SIJ arthrodesis, such as the CT-guided percutaneous technique, whose advantages are reduced blood loss, surgical time, and length of hospitalization [43, 69, 70].
CONCLUSION
SIJ anatomical-area dysfunction is a significant pain generator in LBP patients. Diagnosis is challenging, given the SIJ's complex anatomy, physiology, and variable pain presentation features. A combination of history, physical examination, specific provocative tests, articular block, and imaging is imperative. Treatment may include conservative management, therapeutic blocks (intra- and periarticular) with local anesthetics and corticosteroids, neuro ablation (crio or RFT), and surgery for patients unresponsive to therapies.
AUTHORS’ CONTRIBUTIONS
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| CT | = Computed tomography |
| EMG | = Electromyography |
| FABER | = hip Flexion, Abduction, and External Rotation |
| HLAB27 | = Human leukocyte antigen |
| IASP | = International Association for the Study of Pain |
| ICD | = International Classification of Disease |
| LBP | = Lower Back Pain |
| MG30.02/03 | = Primary/secondary chronic musculoskeletal pain |
| MRI | = Magnetic Resonance Imaging |
| PET | = Positron Emission Tomography |
| PSIS | = Posterior Superior Iliac Spine |
| RDT | = Radiofrequency Denervation Techniques |
| SIJ | = Sacroiliac Joint |
| SPECT | = single-photon emission computed tomography |
| US | = Ultrasound |
| NRS | = Numerical Rating Scale |


