All published articles of this journal are available on ScienceDirect.
Antimicrobial Activity of Lidocaine, Bupivacaine, Mepivacaine and Ropivacaine on Staphylococcus epidermidis, Staphylococcus aureus and Bacillus subtilis
Abstract
Introduction:
Various studies have shown a possible antimicrobial activity of different local anaesthetics, which may affect the results of microbial assessment of biopsies. The purpose of this study was to test the antimicrobial activity of different commonly used anaesthetic agents on Staphylococcus epidermidis, Staphylococcus aureus and Bacillus subtitles to reproduce data and to compare the findings.
Methods:
Local anaesthetics tested were commercially available solutions of lidocaine (Xyloneural®, Xylanaest pur.®), bupivacaine (Bucain®), mepivacaine (Mecain®) and ropivacaine (Naropin®, Ropinaest®).2%, 1%, 0.5%, 0.25% and 0.1% (20, 10, 5, 2.5, 1 mg/ml) dilutions of these local anaesthetics were prepared with sterile 0.9% saline. Bacteria used in this study were Staphylococcus epidermidis, Staphylococcus aureus and Bacillus subtilis. 10 μl of different local anaesthetic dilution placed on thin wafers were added to Mueller Hinton Agar and cultured. After 24 hours, a zone of inhibition around the wafers was evaluated.
Results:
Local anaesthetics in different concentrations did not show any zone of inhibition on Staphylococcus epidermidis, Staphylococcus aureus or Bacillus subtilis.
Conclusion:
In summary, neither lidocaine, bupivacaine, mepivacaine nor ropivacaine showed an antibacterial effect on Staphylococcus epidermidis, Staphylococcus aureus and Bacillus subtilis.
Implications:
Due to these findings this local anaesthetics can be used in daily clinical routine to perform pain free diagnostic procedures in which culture specimens are to be obtained. Due to inconsistent results in prior studies, we recommend to use the lowest concentration possible of the local anaesthetic, also to avoid other possible side effects of local agents.
INTRODUCTION
In clinical practice local anaesthetics are used daily to perform pain free diagnostic procedures. However, various studies have shown a possible antimicrobial activity of different local anaesthetics, which may affect results in microbial assessment of biopsies. The purpose of this study was to test the antimicrobial activity of different commonly used anaesthetic agents on Staphylococcus epidermidis, Staphylococcus aureus and Bacillus subtilis to reproduce data and to compare the findings.
METHODS
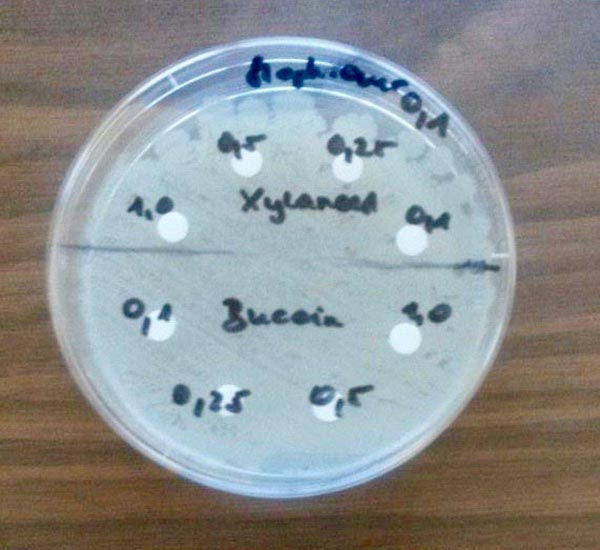
Local anaesthetics tested were commercially available solutions of lidocaine (Xyloneural®, Xylanaest pur.®), bupivacaine (Bucain®), mepivacaine (Mecain®) and ropivacaine (Naropin®, Ropinaest®). 2%, 1%, 0.5%, 0.25% and 0.1% (20, 10, 5, 2.5, 1 mg/ml) dilutions of these local anaesthetics were prepared with sterile 0.9% saline. Bacteria used in this study were Staphylococcus epidermidis, Staphylococcus aureus and Bacillus subtilis. The number of bacteria was prepared to achieve 0.5 McFarland standard and plated. 10 μl of different local anaesthetic dilution placed on thin wafers were added to Mueller Hinton Agar and cultured at 35°C. Wafers without local anaesthetics but 0.9% saline and wafers with ampicillin/sulbactam were used as controls. After 24 hours, a zone of inhibition around the wafers was evaluated, which is a wide ring around the wafer with no bacterial growth.
RESULTS
Local anaesthetics in different concentrations did not show any zone of inhibition on Staphylococcus epidermidis, Staphylococcus aureus or Bacillus subtilis, which means that these bacteria have grown although there was a local anaesthetic (Figs. 1 and 2). Due to these findings the tests were repeated with commercially available undiluted local anaesthetics but with lower densities of microorganisms, according to McFarland standard of 0.25, 0.10 and 0.05 and 100 μl of different local anesthetic solution. After culturing for 24 hours at 35°C there again was no zone of inhibition on tested bacteria and no change in the surrounding bacterial concentration. In summary, 240 combinations of bacterial and local anaesthetics were tested (Table 1).

| Tested local anaesthetics | Mc Farland standard | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Staphylococcus epidermidis |
Staphylococcus aureus |
Bacillus subtilis |
|||||||||||
| conc. | 0,50 | 0,25 | 0,10 | 0,05 | 0,50 | 0,25 | 0,10 | 0,05 | 0,50 | 0,25 | 0,10 | 0,05 | |
| Xyloneural® | 1,0 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm |
| Xylanaest | 0,5 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm |
| pur®. | 0,25 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm |
| 0,1 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | |
| Bucain® | 1,0 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm |
| 0,5 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | |
| 0,25 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | |
| 0,1 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | |
| Mecain® | 1,0 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm |
| 0,5 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | |
| 0,25 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | |
| 0,1 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | |
| Naropin® | 1,0 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm |
| 0,5 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | |
| 0,25 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | |
| 0,1 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | |
| Ropinaest® | 1,0 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm |
| 0,5 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | |
| 0,25 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | |
| 0,1 | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | 0 mm | |
DISCUSSION
In clinical practise local anaesthetics are used daily to perform pain free diagnostic procedures. Considering the literature [1], antimicrobial activity of local anaesthetics could lead to false-negative results in microbial assessment of biopsies. Potential mechanisms of these antimicrobial effects are lysis, increased cell wall permeability and dehydrogenase activity [2]. Various studies conclude that prior to diagnostic biopsies the lowest concentration of local agents should be used or a ring block with additive-free local anaesthetics should be performed [1, 3]. In 2010, Kose and colleagues [4] showed that under in vivo conditions different local anaesthetics did not have any antimicrobial effects. Also Aydin et al. [5] found no antimicrobial properties of ropivacaine but antimicrobial effectiveness of lidocaine and prilocain was observed. The antibacterial activity of lidocaine was negative in a study performed by Berg et al. [3] but they showed that EMLA® has a powerful antibacterial effect. Due to these inconsistent results this present study was conducted to evaluate the antimicrobial effects of different commonly used anesthetic agents on Staphylococcus epidermidis, Staphylococcus aureus and Bacillus subtilis. Neither lidocaine, bupivacaine, mepivacaine nor ropivacaine showed an antibacterial effect. We feel that our large sample size allows us to make a valid conclusion.
CONCLUSION
In summary, neither lidocaine, bupivacaine, mepivacaine nor ropivacaine showed an antibacterial effect on Staphylococcus epidermidis, Staphylococcus aureus and Bacillus subtilis. Due to these findings this local anaesthetics can be used in daily clinical routine to perform pain free diagnostic procedures in which culture specimens are to be obtained. Due to inconsistant results in prior studies we recommend to use the lowest concentration possible of the local anaesthetic, also to avoid other possible side effects of local agents.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No Animals/Humans were used for studies that are base of this research.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


