All published articles of this journal are available on ScienceDirect.
Factors Related to Experiencing Pain in Patients Affected by Chronic Inflammatory Rheumatic Disease During the COVID-19 Pandemic
Abstract
Objective:
To evaluate the effects of the COVID-19 pandemic on the pain experienced by patients with CIRD and to analyze the associated factors.
Methods:
A cross-sectional study was conducted amongst patients with rheumatic diseases using a questionnaire providing information on patients and disease characteristics.
Patients were asked to assess the level of pain they had experienced before and during the pandemic, using a single Visual Analogue Scale (VAS) ranging from 0 (no pain) to 10 (greatest pain).
Statistical Analysis System IBM SPSS Statistics V20.0.0 was used to analyze the study data.
We performed univariate multivariate analysis to search for any related factors to pain perception during the COVID-19 pandemic. Qualitative values were analyzed by the chi2 test. Quantitative values were analyzed by the Student test when the measures were normally distributed or by nonparametric tests (Mann–Whitney U) when the measures were not normally distributed (the Kolmogorov–Smirnov test was used to test normality).
Results:
Amongst the 350 patients who answered the questionnaire online, rheumatoid arthritis represented 62.3%, spondyloarthropathy 34.3%, and undifferentiated CIRD 3.4%. CIRD-related pain was reported by 79.1% of the patients
The level of pain, using the VAS of Pain, increased significantly during the COVID-19 pandemic (4,6 ± 2,8 and 5,4 ± 3 before and during the pandemic; p<0.001).
In the multivariate analysis, the factors causing the pain were: the negative impact of the coronavirus on accessing rheumatology care, the discontinuation of treatment, the disturbed sleep, and the negative psychological impact.
Conclusion:
This survey showed that the COVID-19 pandemic had increased CIRD-related pain in patients. Factors influencing this pain should be considered to help patients cope with their chronic rheumatism in this global health crisis.
1. INTRODUCTION
The outbreak of coronavirus disease in 2019 (COVID-19) was caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, originating in Wuhan, China, where it emerged in late 2019 [1, 2]. The World Health Organization (WHO) declared a “global emergency” on January 30th, 2020. The disease then began spreading rapidly across the globe in February. The WHO declared COVID-19 a pandemic on March 11th [3].
The first known case of COVID-19 in Morocco was detected on March 2nd, 2020, and the first death attributed to the disease occurred on March 10th, 2020 [4].
This pandemic has important implications for patients with rheumatic diseases since most of them are undergoing various immunosuppressive therapies [5-7].
Top scientific organizations have issued recommendations to help rheumatologists care for patients with the rheumatic disease [8-11].
As part of the community of Moroccan rheumatologists, we are concerned about our patients, whether they have stopped their treatment and if they have a worse outcome on their health. We aim to assess the impact of COVID-19 on treatment adherence, to seeing their rheumatologist, and identify the factors related to experiencing pain during the pandemic.
2. MATERIALS AND METHODS
This cross-sectional study was conducted from June 1st to June 30th, 2020 by the Rheumatology Department B at El Ayachi Hospital (national reference center managing rheumatic diseases), with the collaboration of the associations AMRAR (Moroccan Association for Research and Social Aid to Rheumatics) and AMP (Moroccan Association for the Fight Against Rheumatoid Arthritis).
The study included consecutive adult Moroccan patients (aged more than 18 years) suffering from CIRD: Rheumatoid Arthritis (RA), spondyloarthropathy, and undifferentiated CIRD. All patients included in this study had follow-up consultations with a rheumatologist.
The participants of this study were all patients following up in the El Ayachi Hospital (national reference center managing rheumatic diseases) and in the AMRAR and AMPS (Moroccan associations of patients with rheumatoid arthritis and spondyloarthritis) and were reachable by phone. Participants were called by phone, informing them about the purpose and process of the study.
The ethics committee approved the survey approved the survey at the University Mohammed V in Rabat (Faculty of Medicine and Pharmacy), which waived the requirement for informed consent and was conducted in conformity with the ethical principles of research. Answering the questionnaire was considered an agreement to use the responses and all data were analyzed anonymously.
The working group comprised a panel of experts, including three senior rheumatologists and two residents of rheumatology; an expert on infectious diseases and epide-
miology, and an expert in sociology.
We conducted a pilot test with the study committee members, who analyzed the validity of the questionnaire and identified issues that could lead to misunderstandings, and we made the necessary changes until we reached a general agreement. Two rheumatology residents collected the data through the online survey tool “google forms”. The duration of the interview was seven minutes.
2.1. Questionnaire
The questionnaire consists of binary or multiple-choice questions providing information in five sections:
(1) Patients and disease characteristics: age, gender, type of CIRD (RA, spondyloarthropathy, others), duration of disease, current treatment, and comorbidities.
(2) Impact of COVID-19 on seeing a rheumatologist: the impact of COVID-19 on seeing a rheumatologist was estimated through patients’ answers to four questions about difficulties in attending appointments, the nature of these difficulties and the use of telemedicine as an alternative.
(3) Treatment adherence during the pandemic: treatment adherence during the pandemic was assessed by questions about attitudes towards medical treatment (continuation or discontinuation), specification of the discontinued molecule and reasons for discontinuation.
(4) The psychological impact was evaluated by exploring the effects of the containment on negative emotions, quality of sleep, and its impact on psychological health.
(5) Pain caused by CIRD: patients were asked to assess the global pain they felt before and during the pandemic, using a single Visual Analogue Scale (VAS) ranging from 0 (no pain) to 10 (greatest pain).
2.2. Statistics
Statistical Analysis System IBM SPSS Statistics V20.0.0 was used to analyze the survey data.
The qualitative variables were expressed as frequencies. Quantitative values were expressed as mean and standard deviation (SD) or median (interquartile lower, upper).
We performed univariate and multivariate analyses to search for related factors and difficulties in seeing a rheumatologist and investigated pain perception during the pandemic. Qualitative values were analyzed by the chi2 test. Quantitative values were analyzed by the student test when the measures were normally distributed or by a nonparametric test (Mann–Whitney U) when the measures were not normally distributed (Kolmogorov–Smirnov test was used to test normality). Correlation analysis was used to analyze any association between quantitative values. P values of less than 0.05 were considered statistically significant.
3. RESULTS
3.1. Patients and Disease Characteristics
We received answers from 350 patients (68% females, mean age of 46,1 ± 14,4 years) suffering from CIRD (RA (62.3%), spondyloarthropathy (34.3%), and undifferentiated CIRD (3.4%) treated with conventional disease-modifying anti-rheumatic drugs (cDMARDs), and biologic disease-modifying anti-rheumatic drugs (bDMARDs) in respectively 67.4% and 30.6% of cases. Corticosteroids and nonsteroidal anti-inflammatories (NSAIDs) were taken by 39.1% and 33.7% of patients.
Table 1 summarizes the patients and disease characteristics.
3.2. Follow-up and Treatment Adherence
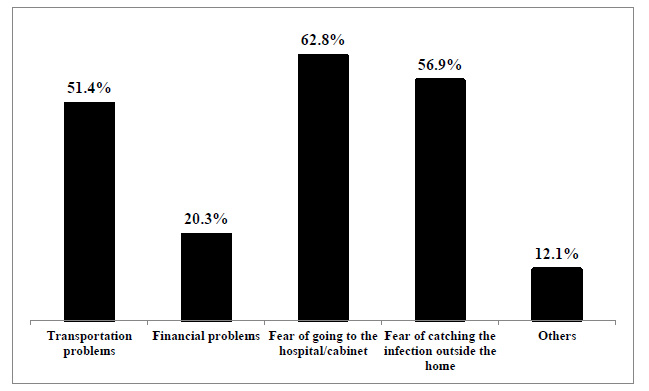
Difficulties in accessing rheumatology appointments were reported by 82.9% of the participants. The fear of going to a medical institution was noted in 62.8% of the cases, among other reasons (Fig. 1). Patients reported that they received rheumatism counseling by their rheumatologists in 65.1% of the cases.
| Patients and Disease Characteristics N=350. | ||
|---|---|---|
| Age (Years)* | 46,1 ± 14,4 [14 - 89] | - |
| Sex | Female/Male (%) | 68/32 |
| CIRD | - | |
| - | RA (%) | 62.3 |
| - | Spondyloarthropathies (%) | 34.3 |
| - | Undifferentiated CIRD (%) | -3.4 |
| Disease Duration (Years)* 10 (4 ; 15) | ||
| Current Treatment (s) (%) | - | |
| - | NSAIDs | 33.7 |
| - | Corticosteroids | 39.1 |
| - | cDMARDs: | 67.4 |
| - | bDMARDs: | 30.6 |
| Comorbidities (%) | - | |
| - | Diabetes | 10.3 |
| - | Cardiovasular diseases | 21.1 |
| - | Pneumopathies | 3.4 |
| - | Nephropathies | 2.9 |
| - | Psychiatric diseases | 5.4 |
RA: Rheumatoid arthritis
NSAIDs: non-steroidal anti-inflammatory drugs
cDMARDs: conventional Disease-modifying anti-rheumatic drugs
bDMARDs: biologic Disease-modifying anti-rheumatic drugs
*Expressed by medians and quartiles
| Drugs | Prevalence of Interruption | Not Found in Pharmacies | The Pharmacy Refuses to Give me the Treatment Without a Recent Prescription | To Avoid the Decrease in Immunity and Therefore to Avoid Catching COVID-19 | I Stopped the Follow-up, and so I Stopped the Treatment... | Other reasons |
|---|---|---|---|---|---|---|
| NSAIDS (%) | 54 | 0 | 27.8 | 74.1 | 44.4 | 27.8 |
| Corticosteroids (%) | 14 | 0 | 14.3 | 92.9 | 57.1 | 50 |
| Methotrexate(%) | 67 | 70.1 | 3 | 10.4 | 16.4 | 22.4 |
| Sulfasalazine (%) | 8 | 0 | 12.5 | 25 | 75 | 100 |
| Synthetic antimalarial (%) | 13 | 69.2 | 0 | 0 | 23.1 | 61.5 |
| Leflunomide (%) | 0 | 0 | 0 | 0 | 0 | 0 |
| bDMARDs (%) | 27 | 0 | 7.4 | 40.7 | 44.4 | 51.9 |
bDMARDs: biologic Disease-modifying anti-rheumatic drugs
According to 50% of the patients, the pandemic has affected their therapeutic compliance. Discontinued drugs were in decreasing order, as follows: synthetic antimalarials (68.4%), NSAIDs (45.8%), methotrexate (43.8%), bDMARDs (25.2%), Sulfasalazine (18.2%) and Corticosteroids (10.2%). Synthetic antimalarials and methotrexate were stopped because of unavailability (69.2% and 70.1%, respectively). Corticosteroids, NSAIDs, and bDMARDs were discontinued due to the fear of an increased risk of COVID-19 infection (92.9%, 74.1%, and 40.7%, respectively).
The causes of treatment interruption are summarized in Table 2.
3.3. The psychological impact of the pandemic
Patients reported that the pandemic negatively affected their mental health in 59.1% of cases. Sleep has been disrupted in 72.6% of patients during the pandemic.
Table 3 summarizes the negative emotions expressed during the containment.
3.4. Pain Experienced During the Pandemic
Pain caused by CIRD during the pandemic was reported by 79.1% of patients.
The levels of pain, using the VAS of pain, were, respectively, at 4,6 ± 2,8 and 5,4 ± 3 before and during the pandemic.
In multivariate analysis, the factors related to experiencing pain are treatment compliance, accessing rheumatology care, disturbed sleep, and the negative psychological impact of the pandemic.
Table 4 summarizes a multivariable analysis of these factors.
| Negative Emotions (%) | - | N = 350 |
|---|---|---|
| Hopelessness | - | 23.7 |
| Anxiety | - | 55.4 |
| Fear | - | 29.7 |
| Frustration | - | 22.9 |
| Loneliness | - | 17.4 |
| Anger | - | 22.6 |
| Powerlessness | - | 24.3 |
| - | P |
|---|---|
| Impact on accessing rheumatology care | 0.05 |
| Impact on therapeutic compliance | <0.001 |
| Disturbed sleep | 0.001 |
| Negative psychological impact | 0.02 |
The link of the survey questionnaire:
https://docs.google.com/forms/d/1tCgpPXP_kRjEgzW65GUl-eYGolL_EEz44CJldNxVsN0/prefill
4. DISCUSSION
This study illustrates the attitudes of Moroccan patients suffering from CIRD during the COVID-19 crisis. It shows the difficulties patients encountered in keeping a regular follow-ups with their rheumatologists, and the high prevalence of discontinued treatments. Experiencing pain during the pandemic would be determined by factors related to the patients and the interruption of monitoring their CIRD.
Most patients found it difficult to see their rheumatologist for many reasons: transportation difficulty, the fear of contracting the coronavirus on their way to the hospital, and an overall fear of catching COVID-19 at the hospital itself.
The discontinued treatments concerned symptomatic (nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids) and conventional and biological disease-modifying antirheumatic drugs. This is alarming and predicts more frequent CIRD outbreaks post-pandemic.
Unjustified discontinuation of long-term CIRD treatment may result in an increased risk of relapse and morbidity in patients with RA and spondyloarthropathy.
The data currently available of patients suffering from rheumatic diseases during the COVID-19 pandemic are reassuring and support the continuation of adequate treatment for better control of CIRD.
National and international recommendations of CIRD emphasize maintaining basic treatments and preventing infection by prioritizing social distancing and stopping immunosuppressants when contracting COVID-19 [8-11].
Aside from the discontinuation of methotrexate, which was mainly caused by the shortage and recurrent problems of availability of this molecule in Morocco, the reasons for discontinuing other drugs were dominated by the fear of patients contracting COVID-19 because of these medications. The shortage of methotrexate in Morocco is a problem that requires national mobilization to avoid overprescribing biological treatments in the context of limited economic resources.
Patients who reported stopping hydroxychloroquine due to the shortage of pharmacies were unaware of a special national initiative to help them acquire hydroxychloroquine.
This survey analyzed the factors associated with experiencing pain during the pandemic. There were also links between a higher level of pain and the difficulties in accessing appropriate care by rheumatologists and the interruption of CIRD medication.
These links confirmed by the analysis should be taken into consideration to improve the management of patients with CIRD.
After having identified the problems encountered by our patients suffering from CIRD, the team of doctors has developed videos in the Moroccan dialect intended for patients. The association’s rheumatologists took turns sending clear messages with concise content, adapting to the different categories of Moroccan patients. We stressed the importance of having patients suffering from CIRD return to routine care by scheduling their appointment as soon as possible with their corresponding rheumatologist. The objective is to assess the activity of rheumatism, adapt the drug treatments, and support the patients to undo any harm caused by the interruption of treatment during the pandemic.
Given the important links discovered between the fear of COVID-19 and the discontinuation of various drugs for rheumatic disease, we sent the patient association documents containing practical and updated medical information on COVID-19, responding to the patients’ concerns, which we have developed under the supervision of the Moroccan Society of Rheumatology (SMR). Furthermore, we asked our fellow psychiatrists to guide us on the appropriate steps to follow to support our patients and deal with the negative psychological consequences of COVID-19.
CONCLUSION
The pandemic has negatively impacted wellbeing, access to care, and treatment compliance in patients with chronic diseases [12-15].
This survey illustrated that the COVID-19 pandemic had exacerbated the experience of pain in CIRD patients. The factors implicated are the impact of the coronavirus on attending follow-up appointments and drug adherence. Factors influencing this pain should be considered to help patients cope with their rheumatism and this global health crisis.
LIST OF ABBREVIATIONS
| VAS | = Visual Analogue Scale |
| SARS-CoV-2 | = Severe Acute Respiratory Syndrome Coronavirus 2 |
| WHO | = World Health Organization |
| SD | = Standard Deviation |
| NSAIDs | = Nonsteroidal Anti-inflammatory Drugs |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The ethics committee approved the survey at the University Mohammed V in Rabat (Faculty of Medicine and Pharmacy).
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All the humans were used in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013 (http://ethics.iit.edu/ecodes/node/3931).
CONSENT FOR PUBLICATION
Waived the requirement for informed consent and was conducted in conformity with the ethical principles of research.
STANDARDS OF REPORTING
STROBE guidelines were used in this study.
AVAILABILITY OF DATA AND MATERIALS
The authors confirm that the data supporting the findings of this study are available within the manuscript.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We are grateful to all patients who participated in this survey and to our colleagues’ rheumatologists who made this survey possible.
Special thanks to all members of the Moroccan association for research and aid to rheumatics (Association Marocaine de Recherche et d'Aide aux Rhumatisants: AMRAR am-rar.org.ma) and the staff of the Moroccan association of patients with rheumatoid arthritis and spondylarthritis (Association Marocaine de Polyarthrite et de Spondyloarthrites) for their precious contribution to this study. Researching rheumatic diseases' impact is essential to develop more specific actions in rheumatology.


