All published articles of this journal are available on ScienceDirect.
Occupational Stress Levels and Coping Strategies among Nurses Working in an Urban Metropolis in North Central Nigeria
Abstract
Background:
Stress is an important psychological concept that can affect health, well-being, and job performance in negative dimensions.
Objective:
This study investigates stress levels and coping strategies among nurses in selected hospitals in North Central Nigeria.
Methods:
The study employed a multistage sample technique method. The study design was descriptive and cross-sectional, using a quantitative strategy. Data analysis was carried out using descriptive and inferential study statistics.
Results:
Finding shows that the minimum age of the participants was 21–30 years, 87% were female, while 41.1% had 1-5 years of working experience. The study revealed that the highest signs and symptoms of stress experienced by the participants included aches and pain (57.5%) and anxiousness (52.5%). The participants experienced moderate stress. The findings revealed that years of experience (r= 0.631, p= 0.000) were observed to be significantly associated with signs and symptoms of stress. The results showed that age (r= -0.243, p= 0.045), religion (r= 0.165, p= 0.032), and experience of memory problems (r= 0.227, p= 0.003) were observed to show significant association with coping strategies.
Conclusion:
Hence, a conducive work environment should be maintained to promote effective nursing care, while periodic stress assessments and management should be implemented by hospital administrators to aid positive coping strategies among nurses.
1. INTRODUCTION
Stress is an important psychological concept that can negatively affect health, well-being, and job performance [1, 2]. Globally, stress is known as one of the harms to human resources causing visible harmful impacts on individual and social life [3]. Job stress is stress that is work-related and it is one of the most important health issues related to human behaviour that can lead to severe mental collapse and different psychological–behavioral disorders [4, 5].
Stress levels experienced among different professions or jobs differ as some professions tend to have higher levels of stress. Nursing is one of the professions with high levels of stress, although specialties and work settings for nurses vary greatly. Nurses are required to provide both medical and emotional support to patients and their families and are expected to hide their negative emotions, which itself is a form of stress [6]. Previous studies have established that the experience of stress at work has unwelcome effects, both on the health and safety of workers and on the health and effectiveness of their organizations [5, 7]. Stress rises when the expectation of a job becomes too much for an employee to handle, resulting in serious mental, physical, and emotional conditions/illnesses, family problems, alcohol, and substance abuse among many workers. In addition, it causes absenteeism from work, accidents at work, and low productivity. The cost of stress is estimated to be millions of dollars every year for employer organizations [7-11].
As an occupation, nursing has a collection of circumstances leading to stress, including a highly demanding job with poor support, rapidly changing circumstances, shortage of resources and staff, and dealing with death and dying. These factors are inherent in nursing and are compounded by environmental factors such as difficult patients and their families, relationships with physicians, low institutional commitment to nursing, and the delivery of poor-quality care. In addition, responsibilities, such as the need to undertake continuing professional development and part-time education and the emotional nature of the job, contribute to the interactive stress and the daily stress of nurses' work [7, 12, 13].
Work-related stress in nursing occurs due to different work factors that place job demands on nurses [3, 14, 15]. Additionally, many of the emotional and physical symptoms that are common among nurses, such as headaches, fatigue, depression, anxiety, and the inability to cope, can be attributed to or exacerbated by stress [16].
Stress in the workplace impairs both the quality and quantity of work and has been a strong contributing factor to accidents or near misses in healthcare settings, such as affecting service delivery [17]. Stress has been linked to low job satisfaction, reduced productivity, and an increase in occupational accidents and health complaints [18]. It is often believed that when a staff is tired, there is bound to be a misuse of equipment which may lead to damage or injury to the staff or the product. Stress has a powerful effect on the mind and, therefore, a significant effect on one's health and well-being. Stress is linked to leading causes of death, including heart disease, suicide, accidents, and cancer [17]. Nurses are individuals with sensitive jobs who deal with the health of society, people and their functioning influences both their health and the health of other society individuals. Hence, the study investigated stress levels and coping strategies among nurses in selected hospitals in an urban metropolis in North Central Nigeria.
2. METHODS
2.1. Research Setting and Design
The study was conducted among nurses working in three selected health facilities in an urban metropolis in North Central Nigeria. A descriptive, cross-sectional, and nonexperimental research design was used.
The target population for the study were nurses working in the three selected hospitals, referred to as Hospitals ‘A’, ‘B’ and ‘C’. Hospital A is a government-owned public general hospital with 15 functioning departments and 250-bed capacity in 250 wards. It is utilised by the majority of people in the study metropolis and its suburb.
Hospital B is the state government hospital that caters to the health of civil servants and other citizens. The hospital has 7 departments and 8 wards, while Hospital C is a children's specialist Hospital with two main wards: pediatric and neonate wards.
Based on records of the hospitals, there were a total of 280 nurses that comprised of 152, 40, and 88 nurses in Hospitals ‘A’, ‘B’ and ‘C’, respectively. From the total population, a sample size of 97 (Hospital A), 26 Hospital, and 57 participants was calculated for Hospitals ‘A’, ‘B’ and ‘C’, respectively. Based on the sample size calculation, a total of 180 participants comprised of 97, 26, and 57 were calculated after factoring 10% attrition. The sample size was calculated using Yamane Taro's formula [19] for the finite population.
2.2. Study Design
A multistage sampling technique involving three stages (simple, random, stratified, and convenience) was used in the study. The first stage involved the selection of the hospitals using simple random sampling. The list of the hospitals in the study metropolis was obtained, each name of the hospitals was written on a strip, and all were put in a container. Three strips were selected from the container, one after the other, without replacement. The second stage involved stratified sampling, where the sample for each hospital was calculated based on the proportion of nurses in each hospital. In the third stage, a convenience sampling technique was used to select participants until the desired number according to stratification was achieved.
Inclusion criteria for the study were; being a professional nurse; working in the selected hospital for at least 12 months; and willingness to participate after clarification of the purpose of the study. Data collection was done daily during each shift between December 2021 and February 2022.
2.3. Instrument and Data Collection
The research instrument that was used for this study was a structured adapted questionnaire designed based on information adapted from similar studies [20-22]. The questionnaire consisted of four sections. Section A focused on participants” demographic characteristics (such as age, gender, ethnicity, religion, marital status, level of education, occupation, and average monthly income).
Section B: involved 24-item questions on signs and symptoms of stress among nurses. Each item had four (4) options with a maximum mean of 4 and a minimum mean of 1; 0-1 was considered no experience of stress; 1.1 – 2.0, little experience, while 2.1 – 3.0 was considered moderate experience and 3.1 – 4.0 was the severe experience of signs and symptoms of stress. Section C also comprised of 24 questions on levels of stress. Each item had four (4) options with a maximum mean of 4 and a minimum mean of 1; 0-1 was measured as no effect; 1.1 - 2.0 was mild effect; 2.1 – 3.0 moderate, while 3.1 – 4.0 was the severe effect. Section D was on stress coping strategies among nurses with 24 items. Each item has four (4) options that were structured to have a four-point rating scale of 1, not experience, 2, usually experience it a little, 3, experience it moderately, and 4, usually experience it a lot. The average mean was 2.5, and a participant with a mean of 2.5 and above was considered to have a good coping strategy, while a mean below 2.5 was considered as having a poor coping strategy.
Data were collected from participants that met the inclusion during various shifts until the required sample size was achieved.
2.4. Data Analysis
The completed questionnaires collected were coded and analysed using Statistical Package for Social Sciences (SPSS) version 25. Data were analysed using descriptive and inferential statistics. Descriptive statistics were used to summarize the data as means, frequencies, and percentages. The inferential statistics used were the one-way analysis of variance (ANOVA), Chi-Square, and Pearson correlation tests. Test for significant differences in means was done using ANOVA test while association was carried out using Chi-square and Pearson correlation tests. The test for the relationship was carried out using chi-square statistics. All analyses were carried out at a 95% confidence interval.
2.5. Ethical Considerations
Before the commencement of the study, ethical approval was obtained from the Ministry of Health, Kwara State, Nigeria, with approval number ERC/MOH/2021/12/013. Moreover, permission was obtained from three selected hospitals. Informed consent was obtained from each participant before participation in the study. Participants’ confidentiality, privacy, and anonymity were maintained throughout the study.
3. RESULTS
3.1. Socio-Demographic Characteristics of the Participants
As shown in Table 1, 57.1% and 35.1% of the study participants in Hospital A and C were within the age range of 21-30 years, while 46.2% were within the age range of 41-50 years in Hospital B. In the three hospitals, over 80% of the participants were females. In addition, 54.1%, 69.2%, and 49.1% of the participants in ‘Hospital A’, ‘Hospital B’ and ‘Hospital C’ had attended at least one training on stress management, respectively.
| Variables | - | Hospital A | Hospital B | Hospital C |
|---|---|---|---|---|
| Age (years) | 21-30 | 56(57.1%) | 10(38.5) | 20(35.1) |
| 31-40 | 17(17.3%) | 3(11.5) | 19(33.3) | |
| 41-50 | 15(15.3%) | 12(46.2) | 12(21.1) | |
| 51-60 | 10(10.2%) | 1(3.8) | 6(10.5) | |
| > 60 | 0(0%) | 0(0%) | 0(0%) | |
| Gender | Male | 11(11.2) | 3(11.5) | 8(14.0) |
| Female | 87(88.8) | 23(88.5) | 49(86) | |
| Ethnicity | Yoruba | 73(74.5) | 24(92.3) | 41(71.9) |
| Igbo | 14(14.3) | 0((0%)) | 6(10.5) | |
| Hausa | 7(7.1) | 2(7.7) | 3(5.3) | |
| Others | 4(4.1) | 0((%)) | 7(12.3) | |
| Marital status | Married | 86(87.8) | 23(88.5) | 50(87.7) |
| Divorced | 6(6.1) | 1(3.8) | 2(3.5) | |
| Widowed | 2(2.1) | 0(0(%)) | 1(1.8) | |
| Separated | 2(2.1) | 0((0%)) | 1(1.8) | |
| Single | 4(4.1 | 2(7.7) | 3(5.3) | |
| Religion | Christianity | 43(43.9) | 11(42.3) | 19(33.33) |
| Islam | 55(56.1) | 15(57.7) | 38(66.7) | |
| Traditional | 0((%)) | 0((0%)) | 0((%)) | |
| Family status | Extended family | 16(16.3) | 5(19.2) | 13(22.8) |
| Nuclear family | 80(81.6) | 21(80.8) | 44(77.2) | |
| Highest qualification | Diploma | 2.0(2.0) | 0((0%)) | 1(1.8) |
| BNSC | 30(30.6) | 14(53.8) | 16(28.1) | |
| MSc | 63(64.3) | 11(42.3) | 36(63.2) | |
| PhD | 3(3.1) | 1(3.8) | 4(7.0) | |
| Rank | Assistant director (ADN) | 4(4.1) | 2(7.7) | 2(3.5) |
| Chief Nursing Officer (CNO) | 14(14.3) | 10(38.5) | 9(15.8) | |
| Principal Nursing Officer (PNO) | 26(26.5) | 0(0%) | 20(35.1) | |
| Senior Nursing Officer (SNO) | 9(9.2) | 2(7.7) | 7(12.3) | |
| Nursing Officer 1 (NO I) | 27(27.6) | 12(46.2) | 12(21.1) | |
| Nursing Officer 11 (NO II) | 17(17.3) | 0(0%) | 7(12.3) | |
| Working experience (years) |
1-5 | 51(52.0) | 9(34.6) | 21(36.8) |
| 6-10 | 14(14.3) | 2(7.7) | 6(10.5) | |
| 11-15 | 21(21.4) | 10(38.5) | 20(35.1) | |
| 16-20 | 3(3.1) | 3(11.5) | 4(7.0) | |
| 21-25 | 3(3.1) | 1(3.8) | 3(5.3) | |
| 26-30 | 3(3.1) | I(3.8) | 3(5.3) | |
| > 30 | 3(3.1) | 0(0%) | 0(0%) | |
| Attended training on stress | Yes | 53(54.1) | 18(69.2) | 28(49.1) |
| No | 45(45.9) | 8(30.8) | 29(50.9) |
3.2. Signs and Symptoms of Stress
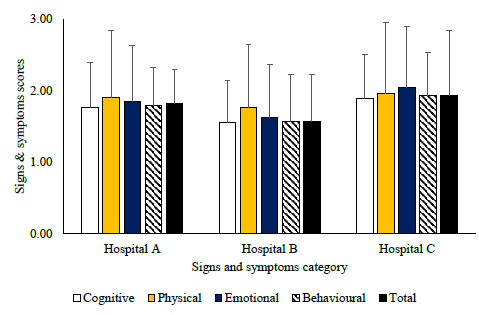
In the three hospitals, participants were observed to have little experience with signs and symptoms of stress in the cognitive, physical and behavioral categories. In the emotional category, little experience of signs and symptoms of stress was also observed for participants in ‘Hospitals A and B’ while participants in ‘Hospital C’ had moderate experience. Generally, the average total experience of signs and symptoms of stress was observed be little across participants in the three hospitals. Average signs and symptoms of stress scores showed significantly higher values in ‘Hospitals A and B’ than that of ‘Hospital C’ (p ≤ 0.05.)Generally, signs and symptoms of stress scores followed the trend among the participants: Hospital C> Hospital A> Hospital B. This observation was irrespective of cognitive, physical, emotional, behavioural, and total signs and symptoms of stress scores (Fig. 1).
Among participants in ‘Hospital A’, a significant association was only observed between a working experience (X2= 35.55, p >.001) and level of signs and symptoms of stress. None of the other demographic characteristics of the participants showed significant association. For participants in ‘Hospital B’ a significant association was only observed for nursing cadre (X2= 34.81, p= 0.003). In the case of participants in ‘Hospital C’, significant was observed between gender (X2= 15.84, p= 0.001), nursing cadre (X2= 34.31, p= 0.03), working experience (X2= 53.64, >.001) and level of signs and symptoms of stress (Table 2).
Table 2.
| Hospital A | Hospital B | Hospital C | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | X2 | p | A | B | C | D | X2 | p | A | B | C | D | X2 | p | |
| Age (years) | ||||||||||||||||||
| 21 – 30 | 10 | 40 | 6 | 0 | 10.18 | .117 | 5 | 4 | 1 | 0 | 11.36 | .252 | 5 | 14 | 1 | 0 | 14.830 | .116 |
| 31- 40 | 5 | 12 | 0 | 0 | 0 | 2 | 0 | 1 | 8 | 8 | 3 | 0 | ||||||
| 41 – 50 | 5 | 7 | 3 | 0 | 4 | 6 | 2 | 0 | 4 | 4 | 2 | 2 | ||||||
| 51 – 60 | 5 | 5 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 3 | 2 | 0 | ||||||
| Gender | ||||||||||||||||||
| Male | 4 | 6 | 1 | 0 | 7.92 | .673 | 0 | 3 | 0 | 0 | 3.39 | .335 | 3 | 1 | 2 | 2 | 15.844 | .001 |
| Female | 21 | 58 | 8 | 0 | 9 | 10 | 3 | 1 | 15 | 28 | 6 | 0 | ||||||
| Marital status | ||||||||||||||||||
| Married | 22 | 56 | 8 | 0 | 3.10 | .812 | 7 | 12 | 3 | 1 | 2.53 | .865 | 15 | 27 | 6 | 2 | 17.577 | .129 |
| Divorced | 2 | 4 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | ||||||
| Separated | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | ||||||
| Single | 1 | 2 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | ||||||
| Religion | ||||||||||||||||||
| Christianity | 8 | 31 | 4 | 0 | 1.97 | .373 | 2 | 7 | 2 | 0 | 3.66 | .301 | 6 | 10 | 9 | 1 | 1.080 | .782 |
| Islam | 17 | 33 | 5 | 0 | 7 | 6 | 1 | 1 | 12 | 19 | 5 | 2 | ||||||
| Family status | ||||||||||||||||||
| Extended | 5 | 11 | 0 | 0 | 7.28 | .122 | 2 | 2 | 1 | 0 | .80 | .850 | 5 | 7 | 1 | 9 | 1.355 | .716 |
| Nuclear | 20 | 53 | 9 | 0 | 7 | 11 | 2 | 1 | 13 | 22 | 7 | 2 | ||||||
| Nursing cadre | ||||||||||||||||||
| ADN | 3 | 0 | 1 | 0 | 15.80 | .201 | 1 | 0 | 0 | 0 | 34.80 | .003 | 0 | 0 | 2 | 0 | 34.310 | .003 |
| CNO | 2 | 10 | 2 | 0 | 0 | 3 | 0 | 0 | 1 | 3 | 3 | 2 | ||||||
| PNO | 9 | 16 | 1 | 0 | 4 | 7 | 2 | 0 | 10 | 9 | 1 | 0 | ||||||
| SNO | 4 | 4 | 1 | 0 | 0 | 0 | 0 | 0 | 2 | 4 | 1 | 0 | ||||||
| NOI | 5 | 19 | 3 | 0 | 2 | 3 | 0 | 0 | 2 | 9 | 1 | 0 | ||||||
| NOII | 2 | 14 | 1 | 0 | 2 | 0 | 0 | 1 | 3 | 4 | 0 | 0 | ||||||
| Working experience (years) | ||||||||||||||||||
| 1-5 | 11 | 35 | 5 | 0 | 35.55 | >.001 | 5 | 3 | 1 | 0 | 17.68 | .280 | 6 | 14 | 1 | 0 | 53.64 | >.001 |
| 6-10 | 0 | 14 | 0 | 0 | 0 | 1 | 0 | 1 | 2 | 3 | 1 | 0 | ||||||
| 11-15 | 9 | 12 | 0 | 0 | 3 | 5 | 2 | 0 | 10 | 8 | 2 | 0 | ||||||
| 16 -20 | 2 | 1 | 1 | 0 | 1 | 2 | 0 | 0 | 0 | 3 | 1 | 0 | ||||||
| 21-25 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 2 | 0 | ||||||
| 26-30 | 0 | 1 | 2 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 2 | ||||||
| > 30 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | ||||||
| Attended any train | ||||||||||||||||||
| Yes | 16 | 32 | 5 | 0 | 1.43 | .490 | 5 | 11 | 2 | 0 | 4.89 | .213 | 10 | 12 | 4 | 2 | 53.64 | >.001 |
| No | 9 | 32 | 4 | 0 | 4 | 2 | 1 | 0 | 8 | 17 | 4 | 0 | ||||||
| Total | 25 | 64 | 9 | 0 | 9 | 13 | 3 | 1 | 18 | 29 | 8 | 2 | ||||||
3.3. Stress Level of the Participants
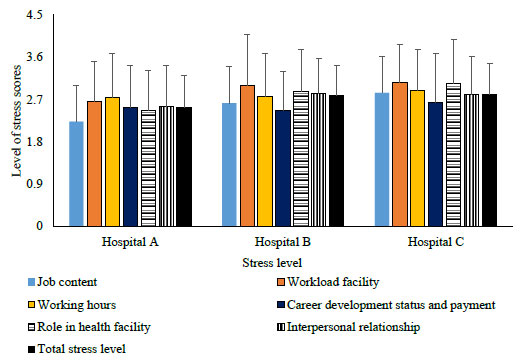
Levels of stress among the participants revealed they were moderately stressed in the categories of job content, working hours, career development status and payment, and interpersonal relationship. This observation was irrespective of the respective hospitals used for investigation. In the categories of workload and facility, participants in ‘Hospital A’ were observed to be moderately stressed, while severe stress was observed for participants in ‘Hospital B and C’. With respect to their role in the health facility, participants in ‘Hospitals A and B’ showed moderate stress, while those in ‘Hospital C’ were severely stressed. Generally, total stress level of the participants revealed followed the trend of Hospital A< Hospital B< Hospital C (Fig. 2). Significantly higher stress level was observed for participants in ‘Hospital C’ than those in ‘Hospitals B and C’ (p≤ 0.005).
Among the demographic profile of participants in ‘Hospital A’, age (X2= 31.80, p>.001), gender (X2= 12.43, p= 0.006), nursing cadre (X2= 58.09, p>.001) and working experience (X2= 45.43, p>.001) showed a significant relationship with stress level. For participants in ‘Hospital B’, none of the demographic characteristics showed a significant association with stress level. In the case of participants in ‘Hospital C’ a significant association was only observed for gender (X2= 8.40, p= 0.038) and family status (X2= 8.95, p= 0.030). Whereas Table 3 indicates the associations of participants’ demographic characteristics with a level of stress among the participants.
3.4. Stress Coping
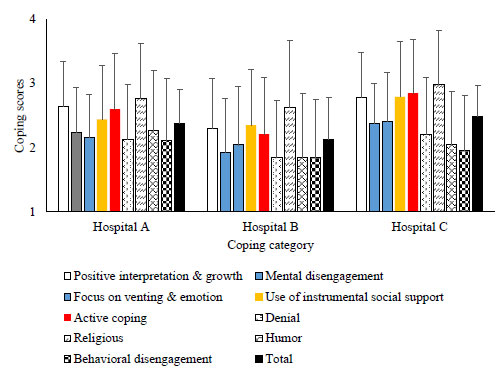
Generally, all the participants moderately utilized strategies including positive interpretation and growth, focus on and venting of emotions, use of instrumental social support, active coping, religious coping and behavioral disengagement in coping with stress. This observation was irrespective of the participants in the respective hospitals. Average total coping scores of the participants in Hospital C>Hospital A> Hospital B’ are shown in Fig. (3). There was no significant difference in coping use among participants in the three hospitals (p≤ 0.05).
Among the participants in ‘Hospital A’, none of the demographic profiles was observed to be significantly associated with stress coping strategies. For participants in ‘Hospital B’, family status (X2= 7.55, p= 0.050) and nursing cadre (X2= 26.10, p= 0.037) showed significant association with stress coping strategy. In the case of participants in ‘Hospital C’, age (X2= 19.91, p= 0.019), gender (X2= 7.99, p= 0.046), nursing cadre (X2= 30.48, p= 0.010) and working experience (X2= 70.57, p< 0.001) showed significant association with stress coping strategy (Table 4).
3.5. Relationship of Signs and Symptoms of Stress and Coping Strategy
Among participants in ‘Hospital A’, signs and symptoms of stress were observed to show a significant positive correlation with stress level (r= 0.313, p= 0.002) and coping strategy (r= 0.267, p= 0.008). In the case of participants in ‘Hospital B’, a significant positive correlation was only observed between the level of stress and coping strategy (r= 0.466, p= 0.002). For participants in ‘Hospital C’, stress level (r= 0.365, p= 0.005) and coping strategy (r= 0.616, p < 0.001) were observed to be significantly positively correlated with stress signs and symptoms (Table 5).
| Hospital A | Hospital B | Hospital C | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | X2 | p | A | B | C | D | X2 | p | A | B | C | D | X2 | p | |
| Age (years) | ||||||||||||||||||
| 21 – 30 | 1 | 23 | 26 | 5 | 31.80 | >.001 | 0 | 3 | 5 | 2 | 2.98 | .811 | 0 | 7 | 11 | 2 | 11.73 | .229 |
| 31- 40 | 0 | 6 | 7 | 4 | 0 | 0 | 2 | 1 | 0 | 4 | 11 | 4 | ||||||
| 41 – 50 | 1 | 4 | 9 | 2 | 0 | 3 | 8 | 1 | 0 | 3 | 6 | 3 | ||||||
| 51 – 60 | 4 | 3 | 2 | 1 | 0 | 0 | 1 | 0 | 1 | 2 | 3 | 0 | ||||||
| Gender | ||||||||||||||||||
| Male | 3 | 3 | 4 | 1 | 12.43 | .006 | 0 | 1 | 2 | 0 | .69 | .708 | 1 | 3 | 2 | 2 | 8.40 | .038 |
| Female | 2 | 33 | 40 | 11 | 0 | 5 | 14 | 4 | 0 | 13 | 29 | 7 | ||||||
| Marital status | ||||||||||||||||||
| Married | 5 | 34 | 37 | 9 | 9.95 | .354 | 0 | 5 | 14 | 4 | 1.68 | .794 | 1 | 13 | 27 | 9 | 769 | .809 |
| Divorced | 0 | 1 | 4 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 2 | 0 | ||||||
| Separated | 0 | 0 | 2 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | ||||||
| Single | 0 | 1 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 0 | ||||||
| Religion | ||||||||||||||||||
| Christianity | 4 | 13 | 21 | 5 | 3.80 | .283 | 0 | 2 | 8 | 1 | 1.077 | .580 | 0 | 5 | 13 | 1 | 3.56 | .313 |
| Islam | 1 | 23 | 23 | 7 | 0 | 4 | 8 | 3 | 1 | 11 | 18 | 8 | ||||||
| Family status | ||||||||||||||||||
| Extended | 1 | 5 | 6 | 4 | 6.53 | .366 | 0 | 3 | 1 | 1 | 5.48 | 0.65 | 1 | 6 | 3 | 3 | 8.95 | .030 |
| Nuclear | 4 | 31 | 38 | 7 | 0 | 3 | 15 | 3 | 0 | 10 | 28 | 6 | ||||||
| Nursing cadre | ||||||||||||||||||
| AND | 3 | 1 | 0 | 0 | 58.09 | >.001 | 0 | 0 | 1 | 0 | 14.42 | .1550 | 0 | 1 | 1 | 0 | 12.69 | .626 |
| CNO | 1 | 3 | 7 | 3 | 0 | 1 | 2 | 0 | 0 | 2 | 4 | 3 | ||||||
| PNO | 0 | 8 | 12 | 6 | 0 | 2 | 10 | 1 | 1 | 4 | 12 | 3 | ||||||
| SNO | 1 | 6 | 2 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 5 | 2 | ||||||
| NOI | 0 | 10 | 14 | 3 | 0 | 0 | 1 | 2 | 0 | 6 | 5 | 1 | ||||||
| NOII | 0 | 8 | 9 | 0 | 0 | 3 | 2 | 0 | 0 | 3 | 4 | 0 | ||||||
| Working experience (years) | ||||||||||||||||||
| 1-5 | 1 | 22 | 24 | 3 | 45.43 | >.001 | 0 | 3 | 4 | 2 | 9.23 | .611 | 0 | 8 | 11 | 2 | 13.78 | .543 |
| 6-10 | 0 | 4 | 7 | 3 | 0 | 0 | 1 | 1 | 0 | 2 | 3 | 1 | ||||||
| 11-15 | 1 | 5 | 9 | 6 | 0 | 1 | 8 | 1 | 1 | 4 | 12 | 3 | ||||||
| 16 -20 | 1 | 1 | 1 | 0 | 0 | 1 | 2 | 0 | 0 | 0 | 3 | 1 | ||||||
| 21-25 | 0 | 3 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 2 | 1 | 0 | ||||||
| 26-30 | 0 | 1 | 2 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 2 | ||||||
| > 30 | 2 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
| Attended any train | ||||||||||||||||||
| Yes | 5 | 19 | 23 | 6 | 4.41 | .221 | 0 | 4 | 12 | 2 | .96 | .618 | 1 | 6 | 16 | 5 | 2.13 | .547 |
| No | 0 | 17 | 21 | 6 | 0 | 2 | 2 | 2 | 0 | 10 | 15 | 4 | ||||||
| Total | 5 | 36 | 44 | 12 | 0 | 6 | 16 | 4 | 1 | 16 | 31 | 9 | ||||||
| Hospital A | Hospital B | Hospital C | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | X2 | p | A | B | C | D | X2 | p | A | B | C | D | X2 | p | |
| Age (years) | ||||||||||||||||||
| 21 – 30 | 2 | 27 | 24 | 2 | 5.02 | .833 | 1 | 4 | 3 | 2 | 9.64 | .380 | 1 | 12 | 7 | 0 | 19.91 | .019 |
| 31- 40 | 1 | 9 | 7 | 0 | 0 | 2 | 1 | 0 | 1 | 11 | 7 | 0 | ||||||
| 41 – 50 | 0 | 10 | 4 | 1 | 0 | 10 | 2 | 0 | 2 | 4 | 3 | 3 | ||||||
| 51 – 60 | 0 | 7 | 3 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 5 | 0 | ||||||
| Gender | ||||||||||||||||||
| Male | 0 | 4 | 6 | 1 | 3.33 | .343 | 0 | 2 | 1 | 0 | 0 | 4 | 2 | 2 | 7.99 | .046 | ||
| Female | 3 | 49 | 32 | 2 | 1 | 14 | 6 | 2 | 7.13 | 0.68 | 4 | 24 | 20 | 1 | ||||
| Marital status | ||||||||||||||||||
| Married | 3 | 49 | 30 | 3 | 6.45 | .694 | 1 | 14 | 6 | 2 | 1.35 | .969 | 4 | 23 | 20 | 3 | 8.61 | .736 |
| Divorced | 0 | 3 | 3 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 2 | 0 | ||||||
| Separated | 0 | 0 | 2 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | ||||||
| Single | 0 | 1 | 3 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | ||||||
| Religion | ||||||||||||||||||
| Christianity | 2 | 27 | 13 | 1 | 3.270 | .352 | 0 | 10 | 6 | 2 | 7.13 | .068 | 2 | 8 | 8 | 1 | 877 | .831 |
| Islam | 1 | 26 | 25 | 2 | 1 | 6 | 1 | 0 | 2 | 20 | 14 | 2 | ||||||
| Family status | ||||||||||||||||||
| Extended | 0 | 10 | 6 | 2 | 3.270 | .352 | 1 | 1 | 2 | 1 | 7.55 | .050 | 0 | 10 | 3 | 0 | 5.77 | .123 |
| Nuclear | 3 | 43 | 32 | 1 | 0 | 15 | 5 | 1 | 4 | 18 | 19 | 3 | ||||||
| Nursing cadre | ||||||||||||||||||
| AND | 0 | 2 | 2 | 0 | 23.19 | .183 | 0 | 1 | 0 | 0 | 26.10 | .037 | 0 | 0 | 2 | 0 | 30.48 | .010 |
| CNO | 0 | 6 | 7 | 1 | 0 | 2 | 1 | 0 | 0 | 2 | 4 | 3 | ||||||
| PNO | 1 | 16 | 9 | 0 | 0 | 11 | 2 | 0 | 2 | 12 | 6 | 0 | ||||||
| SNO | 0 | 4 | 3 | 2 | 0 | 0 | 1 | 0 | 0 | 2 | 5 | 0 | ||||||
| NOI | 2 | 18 | 7 | 0 | 0 | 2 | 2 | 0 | 1 | 6 | 5 | 0 | ||||||
| NOII | 0 | 7 | 10 | 0 | 1 | 0 | 1 | 2 | 1 | 6 | 0 | 0 | ||||||
| Working experience (years) | ||||||||||||||||||
| 1-5 | 1 | 29 | 19 | 1 | 19.42 | .366 | 1 | 3 | 3 | 2 | 17.76 | .276 | 1 | 13 | 7 | 0 | 70.57 | <.001 |
| 6-10 | 1 | 4 | 8 | 1 | 0 | 1 | 1 | 0 | 1 | 3 | 2 | 0 | ||||||
| 11-15 | 1 | 14 | 6 | 0 | 0 | 10 | 0 | 0 | 2 | 12 | 6 | 0 | ||||||
| 16 -20 | 0 | 1 | 2 | 0 | 0 | 1 | 2 | 0 | 0 | 0 | 4 | 0 | ||||||
| 21-25 | 0 | 2 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 3 | 0 | ||||||
| 26-30 | 0 | 2 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 3 | ||||||
| > 30 | 0 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
| Attended any train | ||||||||||||||||||
| Yes | 1 | 31 | 20 | 1 | 1.48 | .687 | 0 | 13 | 4 | 1 | 4.16 | .244 | 2 | 13 | 10 | 3 | 3.31 | .347 |
| No | 2 | 22 | 18 | 2 | 1 | 3 | 3 | 1 | 2 | 15 | 12 | 0 | ||||||
| Total | 3 | 53 | 38 | 3 | 1 | 16 | 7 | 2 | 4 | 28 | 21 | 3 | ||||||
|
Stress Level |
Coping Strategy |
Signs and Symptoms of stress | ||
|---|---|---|---|---|
| Hospital ‘A’ | ||||
| Stress level | Pearson Correlation | 1 | .074 | .313** |
| Sig. (2-tailed) | .471 | .002 | ||
| N | 97 | 97 | 97 | |
| Coping strategy | Pearson Correlation | .074 | 1 | .267** |
| Sig. (2-tailed) | .471 | .008 | ||
| N | 97 | 97 | 97 | |
| Signs & Symptoms of stress | Pearson Correlation | .313** | .267** | 1 |
| Sig. (2-tailed) | .002 | .008 | ||
| N | 97 | 97 | 98 | |
| Hospital ‘B’ | ||||
| Stress level | Pearson Correlation | 1 | -.088 | -.303 |
| Sig. (2-tailed) | .669 | .133 | ||
| N | 26 | 26 | 26 | |
| Coping strategy | Pearson Correlation | -.088 | 1 | .466* |
| Sig. (2-tailed) | .669 | .016 | ||
| N | 26 | 26 | 26 | |
| Signs & Symptoms of stress | Pearson Correlation | -.303 | .466* | 1 |
| Sig. (2-tailed) | .133 | .016 | ||
| N | 26 | 26 | 26 | |
| Hospital ‘C’ | ||||
| Stress level | Pearson Correlation | 1 | .614** | .364** |
| Sig. (2-tailed) | .000 | .005 | ||
| N | 57 | 57 | 57 | |
| Coping strategy | Pearson Correlation | .614** | 1 | .616** |
| Sig. (2-tailed) | .000 | .000 | ||
| N | 57 | 57 | 57 | |
| Signs & Symptoms of stress | Pearson Correlation | .364** | .616** | 1 |
| Sig. (2-tailed) | .005 | .000 | ||
| N | 57 | 57 | 57 | |
| **. Correlation is significant at the 0.01 level (2-tailed). | ||||
4. DISCUSSION
The findings from the study showed that participants experienced a wide range of signs and symptoms of stress. Accordingly, the participants showed a wide range of cognitive, physical, emotional, and behavioural signs and symptoms when confronted with stressful events. The highest cognitive emotional signs and symptoms experienced by participants were anxiousness, worry, being afraid, and difficulty in concentration; these results were similar to the findings of Eldin et al. [23, 24] on stress among nurses in Australia, where concern, feeling of unwell and fear were the highest cognitive-emotional symptoms experienced by the participants. The highest physical and behavioural signs and symptoms experienced by nurses in the current study were aches and pains, frequent cold and flu, chest pain, rapid heartbeat, eating more or less, sleeping more or less and procrastination of tasks. These agreed with the findings of [25] Taj-Eldin et al. [26], where the most common signs and symptoms experienced by participants were headache, pain, irritability, loss of appetite, cold and flu, stomach ache and sweating.
Findings from this study showed that more than half of the participants experienced a moderate level of stress, especially due to frequent night shifts, poor lightening, unsafe environment, no support from senior colleagues, no motivation for further education, conflicting roles with other professions, continuous dealing with client problems and bullying and harassment from patients’ relatives. These findings are similar to the study by Kokoroko and Sanda [27]) who reported that there was a moderate level of stress among nurses who worked at a college hospital in Eritrea. It is crucial for nurses to be healthy and to work in a relatively safe work environment to care for their patients. Moreover, the provision of nursing care requires that the nurse is in the right frame of mind and relaxed to ensure accurate calculation of patient medications, answer her clients' questions professionally, and carry out nursing assessments, among other duties. All these are left undone or done with some errors when the work environment is perceived to be unconducive by the nurse.
It is opined that the major stressors experienced by nurses are problems related to the physical environment, lack of equipment to work with, and being exposed to health and safety hazards. It also showed that problems related to the work environment are associated with occupational stress in nursing [28, 29]. Poor working conditions such as crowded work areas, noise, heat, strong odour, dangerous conditions, and physical strain are also considered potential sources of stress in the workplace [30]. The present study also showed that shifting, especially night duty, caused an increased high level of stress among nurses. A similar observation has been reported elsewhere [31].
In all nine subscales of coping strategies, positive reintegration and religious coping were the most used strategies by the participants, followed by active coping, use of instrumental social support, mental disengagement, focus on and venting of emotion, humor, denial, behavioral engagement. These findings are similar to the conclusion from a previous study conducted by Alfulani et al. [32], which showed that nurses used a variety of coping strategies to deal with workplace stressors. The beneficial effects of employees using coping strategies have been identified to include increase job satisfaction, reduced rate of absenteeism, turn over, and other work-related tensions [3]. Correspondingly, Bhatnagari [1] also agreed with the findings of the current study that regardless of the country, self-control, social support, planful coping, and positive reappraisal were found to be the four most utilised ways of coping.
Findings from the current study revealed that the mean scores for signs and symptoms of stress were observed to be highest for participants in Hospital C, and this observation was irrespective of the subscale considered. This could be due to the fact that the nurses in Hospital C experienced more stress and workload than in Hospitals A and B. Moreover, the difference observed could not be far from the fact that the hospitals are autonomous, having control over their mode of operation in the different or peculiar work environment and management, which to a large extent, contribute to the stress experienced by nurses. Earlier investigators have reported similar observations [28, 33]. In the current study, there was a significant relationship between age, gender, and year of experience of participants, and signs and symptoms. This is similar to the findings of Manzar et al. [34, 35], which revealed that signs and symptoms of stress could be influenced by the age and gender of the participants, although this was not in agreement with the study of Devebakan [6] where age and gender were not related to signs and symptoms of stress.
In this study, the highest stress level was reported by nurses from Hospital C, followed by Hospital B and then nurses from Hospital A. The highest stress level reported by nurses from Hospital C could be linked to the fact that Hospital C is the only pediatric specialty hospital in the state receiving referrals from all other hospitals for pediatric cases. Moreover, by virtue of its location, it is situated at the centre of the Ilorin metropolis. This makes it more accessible to customers of health care services. In view of the above, it can be deduced that Hospital C experiences a higher influx of patients than the other two hospitals. Moreover, the shortage of staff resulting in inadequate nurses to cover the units adequately may be a reason for the frequently stressful conditions. This was in line with a study done in Jordan which showed that the differences in the level of stress experienced by nurses showed that the lack of enough staff to cover all units was the most stressful event perceived by the nurses [29].
The lowest level of stress reported by nurses from Hospital A could be due to the fact that the scope of practice of the nurses is narrower when compared with others. It is the only General Hospital among the hospitals studied and cannot be compared with others in terms of funding, the quantity of manpower, specializations, and better conditions of service. It is reported [35] that adequate funding, enough manpower, and better condition of service can reduce the level of stress experienced by nurses. Al-Aameri [36] stated that adequate knowledge of stress and its coping strategies could enhance the appropriate use of coping strategies by nurses in the management of stress. The current study also showed that there exists a relationship between participants’ age, gender, years of experience, and stress level. This observation corroborates the reports of earlier investigators [6, 8, 36] who indicated that stress levels can be influenced by age, gender, shift work, and work experience.
5. LIMITATIONS OF THE STUDY
The study was cross-sectional in approach; thus, participants were not investigated over a period of time. In addition, the findings are within the context of the study location, thus may not be generalised. However, these limitations did not in any way invalidate the study findings.
6. CONCLUSION
This research study has highlighted the significant results of the effect of stress and coping strategies among nurses in selected hospitals in Ilorin, Kwara State. The study reveals the different physical and behavioural signs and symptoms of stress among nurses. A moderate level of stress was experienced by the majority of the participants, and positive coping strategies utilized include positive reintegration, religious coping, active coping, use of instrumental social support, mental disengagement, focus on and venting of emotion, humor, denial and behavioral engagement. There was a significant relationship between participants’ socio-demographic characteristics (working experience, gender, nursing cadre) and signs and symptoms of stress. Furthermore, the results also indicated a significant relationship between stress level and participants’ age, gender, cadre, family status, and work experience
Hospital administrators and other relevant stakeholders in the health sector should ensure the provision of necessary infrastructures and ensure that the work environment is safe and conducive for nurses and other healthcare professionals to work. Moreover, periodic and continuous training on stress management should be ensured to reduce the effects of stress experienced by nurses, thereby promoting positive coping strategies as well as the provision of quality nursing care and practice.
LIST OF ABBREVIATIONS
| SPSS | = Statistical Package for Social Sciences |
| ANOVA | = One-way Analysis of Variance |
| ADN | = Assistant Director |
| CNO | = Chief Nursing Officer |
| PNO | = Principal Nursing Officer |
| SNO | = Senior Nursing Officer |
| NO I | = Nursing Officer 1 |
| NO II | = Nursing Officer 11 |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was obtained from the Ministry of Health, Kwara State, Nigeria with approval number ERC/MOH/2021/12/013.
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. This research was conducted on humans in accordance with the Helsinki Declaration of 1975, as revised in 2013 (http://ethics.iit.edu/ecodes/node/3931).
CONSENT FOR PUBLICATION
Informed consent was obtained from each participant before participation in the study.
STANDARDS FOR REPORTING
STROBE guidelines and methodology were followed.
AVAILABILITY OF DATA AND MATERIALS
The datasets used and/or analysed during the current study are available from the corresponding author [O.A] on reasonable request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors would like to acknowledge Afe Babalola University, Ado-Ekiti, Ekiti State Nigeria for the provision of research (publication) grant for this study. Special thanks to the hospitals and nurses who participated in the study.


